Introduction: Navigating the Global Market for dental implants with bone loss
Navigating the complexities of dental implants in the context of bone loss is critical for B2B buyers in the dental industry. As global demand for effective tooth replacement solutions continues to rise, understanding the intricacies of dental implants becomes increasingly vital. For many patients, especially in regions like Africa, South America, the Middle East, and Europe, addressing bone loss is not just a cosmetic concern; it is essential for restoring functionality and overall health.
This guide offers a comprehensive overview of dental implants with bone loss, detailing various types of implants, including mini implants and zygomatic implants, as well as innovative solutions such as bone grafts and sinus lifts. We will explore the materials commonly used in these implants and the manufacturing and quality control processes that ensure their efficacy and safety.
Furthermore, understanding the costs associated with these procedures, alongside insights into reliable suppliers and market trends, empowers international B2B buyers to make informed sourcing decisions. Whether you are a dental clinic seeking to expand your offerings or a supplier aiming to meet the specific needs of your clientele, this guide is designed to provide actionable insights that enhance your competitive edge in the global marketplace.
By leveraging this information, dental professionals can better navigate the challenges posed by bone loss, ensuring optimal patient outcomes and satisfaction.
Understanding dental implants with bone loss Types and Variations
| Type Name | Key Distinguishing Features | Primary B2B Applications | Brief Pros & Cons for Buyers |
|---|---|---|---|
| Standard Dental Implants | Requires adequate bone density; titanium post for stability. | General dental practices, implant clinics. | Pros: Highly effective, long-lasting. Cons: Requires sufficient bone, may need grafting. |
| Mini Dental Implants | Smaller in size; less invasive; suitable for lower bone density. | Clinics with patients needing immediate solutions. | Pros: Quick recovery, minimal bone requirement. Cons: Less stability, potential for marginal bone loss. |
| Bone Grafts | Augments existing bone using donor or synthetic materials. | Oral surgeons, advanced dental practices. | Pros: Restores bone density for implants. Cons: Longer procedure, potential complications. |
| Zygomatic Implants | Anchored in the cheekbone; no grafting required. | Specialized clinics for severe bone loss. | Pros: Ideal for patients with extensive upper jaw bone loss. Cons: More complex procedure, higher cost. |
| Sinus Lifts | Raises sinus membrane to allow bone grafting in upper jaw. | Oral and maxillofacial surgery centers. | Pros: Expands treatment options for upper jaw implants. Cons: Surgical risks, longer recovery time. |
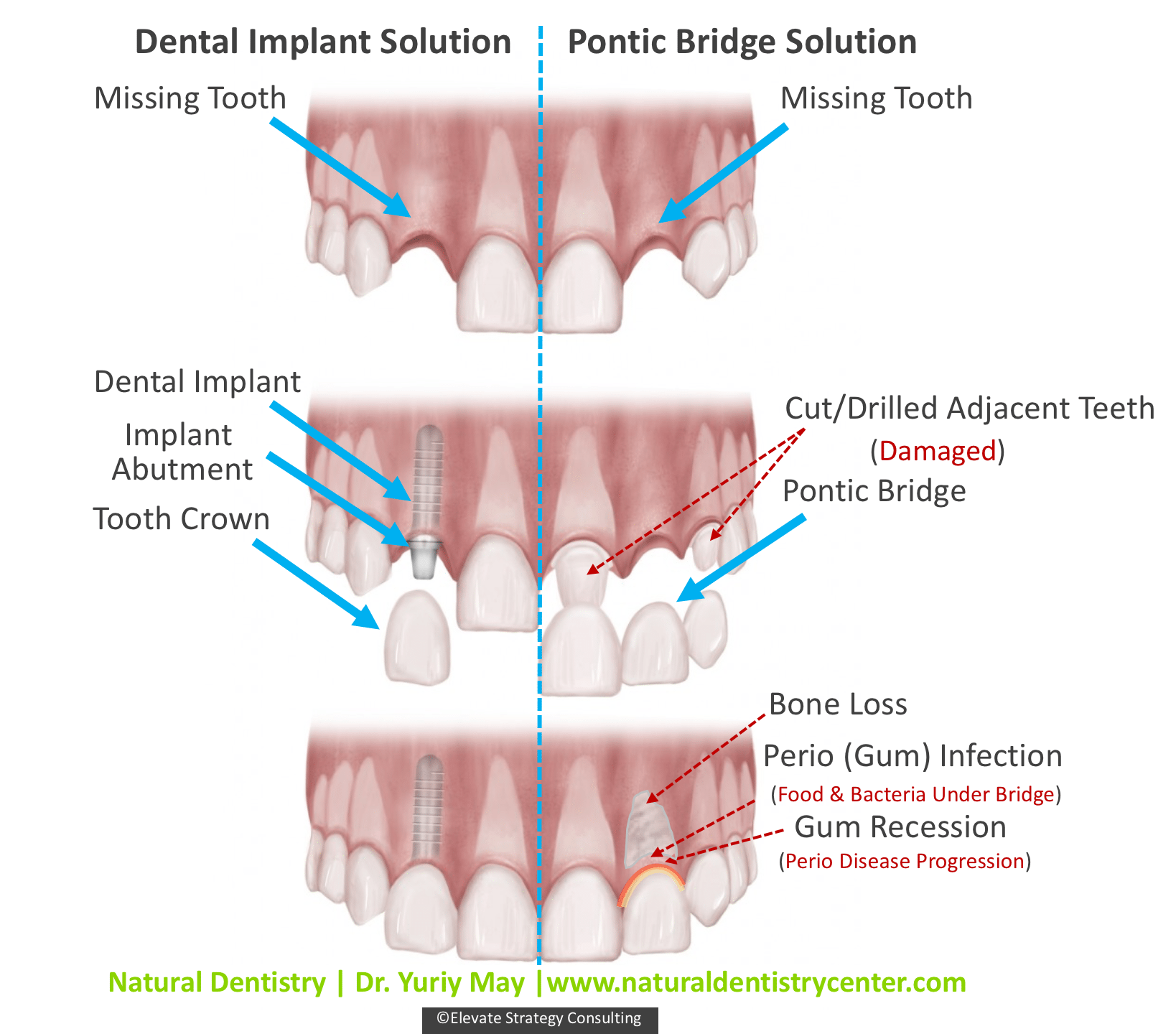
Standard Dental Implants
Standard dental implants are the most common type, featuring a titanium post that is surgically placed into the jawbone. They require a certain level of bone density for successful placement, making them unsuitable for patients with significant bone loss. B2B buyers should consider the need for pre-implant evaluations and potential bone grafting procedures, which can increase overall costs and treatment time.
Mini Dental Implants
Mini dental implants are a smaller version of standard implants, designed for cases with limited bone density. They are less invasive and can often be placed without the need for grafting. For B2B buyers, these implants offer a quicker solution for patients who may require immediate tooth replacement. However, it’s essential to weigh their reduced stability against potential long-term outcomes.
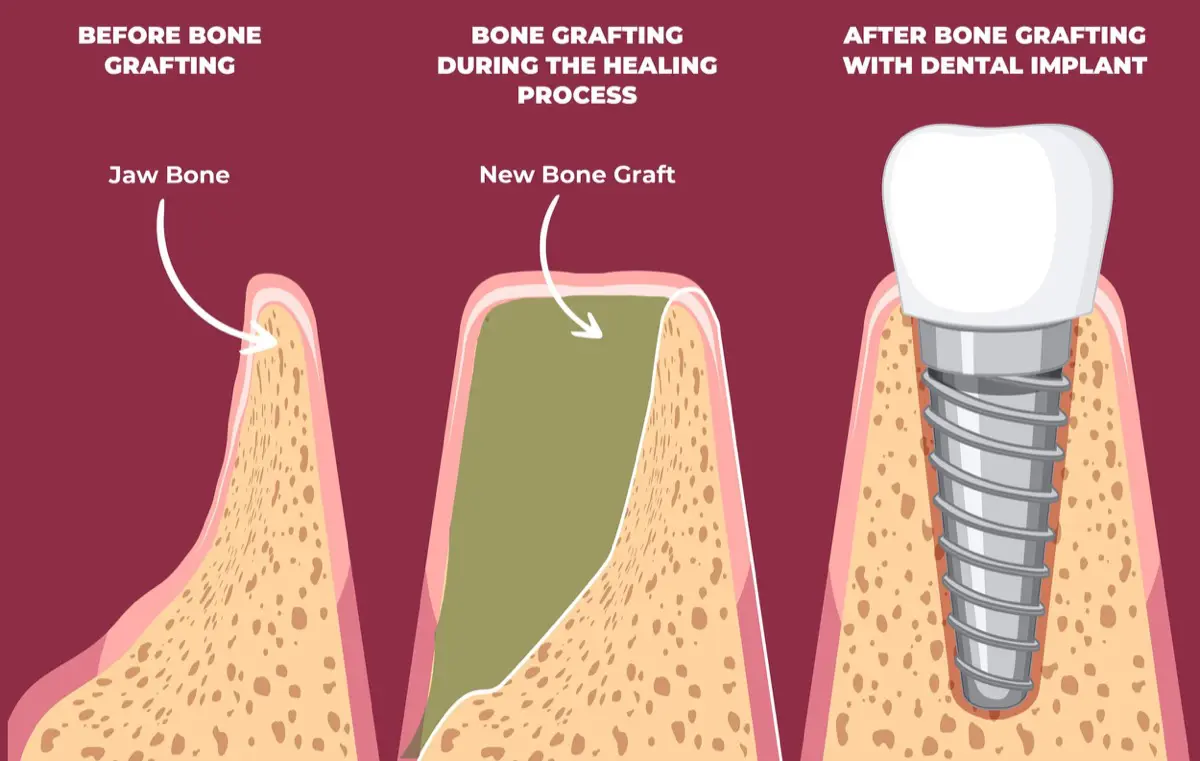
Bone Grafts
Bone grafting involves augmenting the jawbone with material from the patient, a donor, or synthetic options to create a stable base for implants. This procedure is crucial for patients with significant bone loss. B2B buyers should be aware of the complexities involved, including the need for specialized surgical expertise and potential complications, which may affect the overall treatment timeline and costs.
Zygomatic Implants
Zygomatic implants are anchored in the cheekbone, providing an alternative for patients with severe upper jaw bone loss who cannot undergo traditional grafting. These implants are advantageous for B2B buyers looking to offer solutions in cases where other implant options have failed. However, they require specialized surgical skills and can be more expensive due to their complexity.
Sinus Lifts
A sinus lift is a surgical procedure that raises the sinus membrane to allow for bone grafting in the upper jaw, facilitating the placement of implants in patients with bone loss. For B2B buyers, this option expands the range of treatable cases and can significantly enhance patient outcomes. However, the procedure carries surgical risks and may require a longer recovery period, which should be factored into patient consultations and treatment planning.
Related Video: Dental Implants 101: What You NEED to Know! Part 3 (Everything Bone Grafting)
Key Industrial Applications of dental implants with bone loss
| Industry/Sector | Specific Application of dental implants with bone loss | Value/Benefit for the Business | Key Sourcing Considerations for this Application |
|---|---|---|---|
| Dental Clinics | Bone grafting and zygomatic implants | Expanded patient base and treatment options | Quality of materials, regulatory compliance, supplier reliability |
| Oral and Maxillofacial Surgery | Reconstruction procedures using implants | Enhanced surgical outcomes and patient satisfaction | Availability of advanced surgical technologies, training for staff |
| Dental Laboratories | Custom implant fabrication for complex cases | Increased precision and reduced surgery time | Compatibility with existing systems, material sourcing, and turnaround time |
| Health Insurance Providers | Coverage for dental implants procedures | Improved patient retention and satisfaction | Understanding of regional regulations, partnership with dental professionals |
| Medical Device Manufacturers | Development of innovative implant solutions | Competitive advantage through product differentiation | Research and development capabilities, adherence to international standards |
Dental Clinics
Dental clinics play a crucial role in the application of dental implants for patients experiencing bone loss. By offering procedures such as bone grafting and zygomatic implants, clinics can cater to a wider range of patients, including those with severe bone loss. This not only expands the clinic’s patient base but also enhances treatment options. When sourcing implants, clinics must prioritize the quality of materials and ensure compliance with local regulations to maintain patient safety and trust.
Oral and Maxillofacial Surgery
In oral and maxillofacial surgery, dental implants are often utilized for reconstruction procedures. These implants can restore functionality and aesthetics for patients suffering from significant bone loss due to trauma or disease. The integration of advanced implant techniques can lead to improved surgical outcomes and higher patient satisfaction rates. Surgeons should consider the availability of advanced surgical technologies and ensure that their teams are adequately trained to handle complex cases.
Dental Laboratories
Dental laboratories are essential in custom implant fabrication, particularly for complex cases involving bone loss. By leveraging advanced technologies, laboratories can create highly precise implants that fit individual patient anatomies, thereby reducing surgery time and improving outcomes. When sourcing materials, laboratories need to ensure compatibility with existing systems and maintain a quick turnaround time to meet the demands of dental practices.
Health Insurance Providers
Health insurance providers can benefit from covering dental implant procedures, particularly for patients with bone loss. By offering coverage for these treatments, providers can enhance patient retention and satisfaction while addressing the increasing demand for dental health services. Understanding regional regulations and forming partnerships with dental professionals are critical for insurers to effectively tailor their policies and meet the needs of their members.
Medical Device Manufacturers
Medical device manufacturers are at the forefront of developing innovative implant solutions for patients with bone loss. By focusing on research and development, these companies can create differentiated products that meet the specific needs of this market segment. Adherence to international standards and regulations is vital for manufacturers to ensure product safety and efficacy, which will ultimately provide a competitive advantage in the global marketplace.
Related Video: Guided bone regeneration with simultaneous implant placement
Strategic Material Selection Guide for dental implants with bone loss
When selecting materials for dental implants designed for patients with bone loss, it is essential to consider the unique properties and performance characteristics of various materials. Here, we analyze four common materials used in dental implants, focusing on their key properties, advantages, disadvantages, and considerations for international B2B buyers.
Titanium
Key Properties: Titanium is renowned for its excellent biocompatibility, corrosion resistance, and strength-to-weight ratio. It can withstand the pressures exerted during chewing and is resistant to the acidic environment of the oral cavity.
Pros & Cons: Titanium implants are highly durable and have a long track record of success in dental applications. However, they can be more expensive than other materials, and the manufacturing process can be complex due to the need for precision machining.
Impact on Application: Titanium is compatible with various bone grafting techniques, making it suitable for patients with significant bone loss. Its ability to osseointegrate effectively with bone is critical for long-term stability.
Considerations for International Buyers: Buyers in regions like Africa and South America should ensure that titanium implants comply with international standards such as ASTM F136. Additionally, understanding local regulations regarding medical devices is crucial for successful market entry.
Zirconia
Key Properties: Zirconia is a ceramic material known for its aesthetic appeal and high strength. It possesses excellent fracture toughness and is resistant to wear, making it suitable for dental applications.
Pros & Cons: The primary advantage of zirconia implants is their tooth-like appearance, which is especially important for anterior restorations. However, they can be less durable than titanium under high stress and are generally more expensive.
Impact on Application: Zirconia implants are ideal for patients concerned about aesthetics, particularly in visible areas. Their non-metallic nature makes them a good choice for patients with metal allergies.
Considerations for International Buyers: Compliance with standards such as ISO 6872 is essential for zirconia implants. Buyers in Europe, particularly in France, should also be aware of the CE marking requirements for dental products.
Polyether Ether Ketone (PEEK)
Key Properties: PEEK is a high-performance polymer that offers excellent mechanical properties, including strength and flexibility. It is resistant to chemicals and has a lower density compared to metals.
Pros & Cons: PEEK implants are lightweight and can be manufactured with less complexity than metal implants. However, they may not provide the same level of osseointegration as titanium, which could impact long-term stability.
Impact on Application: PEEK is suitable for patients who require a less invasive procedure and have moderate bone loss. Its flexibility allows for better adaptation to the bone structure.
Considerations for International Buyers: Buyers should ensure PEEK implants meet relevant standards such as ASTM F2026. Understanding the regulatory landscape in the Middle East is also important, as some countries may have specific requirements for polymer-based implants.
Cobalt-Chromium Alloys
Key Properties: Cobalt-chromium alloys are known for their high strength, wear resistance, and corrosion resistance. They are often used in dental applications where durability is paramount.
Pros & Cons: These alloys provide excellent mechanical properties and are less prone to fracture compared to other materials. However, they can be more challenging to manufacture and may cause allergic reactions in some patients.
Impact on Application: Cobalt-chromium implants are particularly suitable for patients with severe bone loss, as they can provide robust support for prosthetic teeth. Their strength makes them ideal for load-bearing applications.
Considerations for International Buyers: Compliance with standards such as ASTM F75 is crucial for cobalt-chromium alloys. Buyers from South America should be aware of local regulations regarding the importation of metal-based medical devices.
| Material | Typical Use Case for dental implants with bone loss | Key Advantage | Key Disadvantage/Limitation | Relative Cost (Low/Med/High) |
|---|---|---|---|---|
| Titanium | Standard dental implants for patients with bone loss | Excellent biocompatibility and durability | Higher cost and complex manufacturing | High |
| Zirconia | Aesthetic implants for visible areas | Tooth-like appearance | Less durable under high stress | High |
| Polyether Ether Ketone (PEEK) | Less invasive implants for moderate bone loss | Lightweight and flexible | Lower osseointegration potential | Medium |
| Cobalt-Chromium Alloys | Load-bearing implants for severe bone loss | High strength and wear resistance | Potential allergic reactions | Medium |
This strategic material selection guide provides international B2B buyers with essential insights into the various materials available for dental implants designed for patients with bone loss. Understanding the properties, advantages, and limitations of each material will aid in making informed purchasing decisions that align with market demands and regulatory requirements.
In-depth Look: Manufacturing Processes and Quality Assurance for dental implants with bone loss
The manufacturing of dental implants designed for patients with bone loss involves a meticulous process that guarantees both functionality and safety. This section outlines the critical stages of the manufacturing process, quality control (QC) standards, and actionable insights for international B2B buyers.
Manufacturing Process
The manufacturing of dental implants with bone loss considerations typically involves the following key stages:
1. Material Preparation
The choice of materials is crucial for the success of dental implants. Common materials include titanium and zirconia, known for their biocompatibility and strength. The preparation phase includes:
Illustrative Image (Source: Google Search)
- Sourcing: Ensure materials meet international standards for medical devices. For example, titanium should comply with ASTM F136.
- Cleaning and Sterilization: Materials must undergo rigorous cleaning to remove any contaminants. This is often performed using ultrasonic cleaning and autoclaving.
2. Forming
This stage involves shaping the implant components through various techniques:
- CNC Machining: Computer Numerical Control (CNC) machining is widely used to achieve precise dimensions and surface finishes. This process allows for the creation of complex geometries necessary for effective osseointegration.
- Additive Manufacturing: Also known as 3D printing, this technique is gaining traction for creating porous structures that promote bone growth around the implant.
3. Assembly
The assembly phase focuses on integrating various components of the dental implant system:
- Component Assembly: This includes attaching the abutment to the implant body. Care must be taken to ensure proper torque settings to avoid loosening.
- Quality Assurance Checks: Throughout the assembly process, visual inspections and functional tests are conducted to ensure that components fit correctly and meet design specifications.
4. Finishing
Finishing processes enhance the implant’s surface properties, which is vital for long-term success:
- Surface Treatment: Techniques such as sandblasting, acid etching, or coating with hydroxyapatite are applied to improve osseointegration.
- Final Sterilization: Before packaging, implants undergo terminal sterilization to eliminate any microbial contamination.
Quality Assurance
Quality assurance is integral to the manufacturing of dental implants, especially for those designed for patients with bone loss. Compliance with international standards and rigorous QC checkpoints are essential.
Relevant International Standards
- ISO 9001: This standard ensures that organizations meet customer and regulatory requirements while maintaining consistent quality.
- ISO 13485: Specific to medical devices, this standard emphasizes the quality management systems that manufacturers must implement.
- CE Marking: Required for products sold in the European Economic Area, indicating that the implant meets EU safety and performance requirements.
- FDA Approval: For markets such as the United States, FDA approval is critical, ensuring that the implant is safe and effective for use.
QC Checkpoints
Quality control checkpoints are categorized into several stages:
- Incoming Quality Control (IQC): Materials are inspected upon receipt to ensure they conform to specifications.
- In-Process Quality Control (IPQC): Continuous monitoring during the manufacturing process, including dimensional checks and process parameter controls.
- Final Quality Control (FQC): Final inspections are conducted before packaging, including functional testing and visual inspections.
Common Testing Methods
- Mechanical Testing: Tensile, compressive, and fatigue tests assess the mechanical properties of the implant.
- Biocompatibility Testing: Ensures that the materials used do not provoke adverse reactions when implanted in the body.
- Sterility Testing: Validates that the sterilization processes effectively eliminate microbial contamination.
Verifying Supplier QC
B2B buyers should be proactive in verifying the QC processes of their suppliers. Here are several strategies to ensure compliance and quality:
- Conduct Supplier Audits: Regular audits of suppliers can help verify their compliance with international standards and internal QC processes.
- Request Quality Reports: Suppliers should provide documentation detailing their QC processes, including results from testing and inspections.
- Engage Third-Party Inspectors: Utilizing independent third-party inspectors can provide an unbiased assessment of the supplier’s quality management system.
QC and Certification Nuances for International B2B Buyers
For buyers from regions such as Africa, South America, the Middle East, and Europe, it’s essential to understand the nuances of certification and quality control:
- Regional Regulations: Familiarize yourself with local regulations that may affect the importation and sale of dental implants, such as ANVISA in Brazil or COFEPRIS in Mexico.
- Cultural Sensitivities: Be aware of cultural differences in business practices, which may impact negotiations and partnerships.
- Supply Chain Logistics: Assess the logistical challenges of sourcing implants from international suppliers, including shipping times and customs regulations.
Conclusion
Understanding the manufacturing processes and quality assurance protocols for dental implants designed for patients with bone loss is vital for B2B buyers. By focusing on reputable suppliers that adhere to international standards and implementing robust verification strategies, buyers can ensure they are sourcing high-quality products that will meet the needs of their patients effectively.
Comprehensive Cost and Pricing Analysis for dental implants with bone loss Sourcing
In the sourcing of dental implants for patients with bone loss, understanding the comprehensive cost structure is essential for international B2B buyers. This analysis provides insight into the various cost components, price influencers, and practical tips for negotiation and cost-efficiency.
Cost Components
-
Materials: The primary materials used in dental implants include titanium or zirconia for the implant body, and various biocompatible materials for bone grafts (e.g., hydroxyapatite). The choice of materials directly affects the cost, with titanium typically being more expensive due to its superior strength and compatibility.
-
Labor: Labor costs encompass the expertise required for surgical procedures as well as the manufacturing of the implants. Skilled labor is essential for both the surgical implantation and the production of high-quality implants, which can vary significantly between regions.
-
Manufacturing Overhead: This includes costs associated with facilities, utilities, and administrative expenses. Companies that produce implants in regions with higher operational costs, such as Western Europe, may have higher overhead compared to those in developing markets.
-
Tooling: The initial setup costs for manufacturing tools and equipment can be significant. Advanced technologies such as CAD/CAM systems for custom implant production can increase tooling costs but may also lead to better patient outcomes and lower long-term expenses.
-
Quality Control (QC): Rigorous QC processes are vital to ensure implant safety and efficacy. Costs associated with testing, certification, and compliance with international standards (e.g., ISO 13485) can add to the overall price.
-
Logistics: Transportation costs are influenced by distance, shipping methods, and customs regulations. International buyers should factor in these costs, especially when importing implants from regions with stringent regulations.
-
Margin: Supplier margins can vary widely based on competition and market demand. Suppliers may adjust margins based on their market positioning, brand reputation, and the perceived value of their products.
Illustrative Image (Source: Google Search)
Price Influencers
-
Volume/MOQ: Larger orders typically lead to discounts. Buyers should negotiate minimum order quantities (MOQs) to optimize costs while ensuring sufficient inventory.
-
Specifications/Customization: Custom implants designed for specific patient needs can significantly increase costs. Standardized options are usually more cost-effective.
-
Material Quality/Certifications: Implants with higher quality certifications tend to command premium prices. Buyers should assess whether the additional cost for certified products is justified by the quality and expected outcomes.
-
Supplier Factors: The reputation and reliability of suppliers can influence pricing. Established suppliers with proven track records may charge more but offer better guarantees and support.
-
Incoterms: Understanding shipping terms is crucial. Terms such as FOB (Free On Board) or CIF (Cost, Insurance, and Freight) can affect overall costs and responsibilities during shipping.
Buyer Tips
-
Negotiation: Always negotiate prices and terms. Suppliers may have flexibility in pricing, especially for larger orders or long-term contracts.
-
Cost-Efficiency: Consider the Total Cost of Ownership (TCO), which includes initial costs, maintenance, and potential failure rates. Investing in higher-quality implants may reduce long-term costs associated with replacements or complications.
-
Pricing Nuances: International buyers should be aware of currency fluctuations and their impact on pricing. Additionally, understanding local market dynamics can provide leverage during negotiations.
-
Regional Considerations: Buyers from Africa, South America, the Middle East, and Europe must consider regional regulations and market conditions that could affect pricing and availability. For instance, European suppliers may offer higher quality but at a premium price compared to emerging markets.
Disclaimer
Prices for dental implants with bone loss can vary significantly based on the above factors. This analysis provides indicative pricing insights, and actual costs may differ based on specific buyer conditions and market fluctuations. Always consult with multiple suppliers to obtain accurate quotes tailored to your needs.
Spotlight on Potential dental implants with bone loss Manufacturers and Suppliers
This section looks at several manufacturers active in the ‘dental implants with bone loss’ market. This is a representative sample for illustrative purposes; B2B buyers must conduct extensive due diligence before any transaction. Information is synthesized from public sources and general industry knowledge.
Essential Technical Properties and Trade Terminology for dental implants with bone loss
Essential Technical Properties
Understanding the technical properties of dental implants designed for patients with bone loss is crucial for B2B buyers in the dental industry. Here are some key specifications to consider:
-
Material Grade
Dental implants are primarily made from titanium or zirconia. Titanium is favored for its strength, biocompatibility, and ability to osseointegrate (bond with bone). Zirconia, while aesthetically pleasing, may not offer the same level of strength as titanium. Selecting the appropriate material ensures durability and reduces the risk of implant failure, which is vital for maintaining patient satisfaction and reducing long-term costs. -
Surface Roughness
The surface texture of dental implants affects osseointegration. Implants with a roughened surface (measured in micrometers) enhance bone attachment compared to smooth surfaces. This property is particularly important for patients with compromised bone density, as it can significantly impact the stability and longevity of the implant. -
Diameter and Length
The dimensions of the implant are critical for stability, especially in cases of bone loss. Standard diameters range from 3.0 mm to 5.0 mm, while lengths can vary from 8 mm to 16 mm. Customizing these dimensions based on individual patient needs and available bone can help prevent complications and ensure a successful outcome. -
Load-Bearing Capacity
This refers to the amount of force an implant can withstand during chewing and speaking. For patients with bone loss, selecting implants with a higher load-bearing capacity can minimize the risk of fracture or failure, making it essential for B2B buyers to understand the mechanical properties of the implants they are sourcing. -
Implant Design
The design can vary significantly, with options like tapered or cylindrical shapes. Tapered designs are often preferred for patients with limited bone due to their ability to distribute forces more evenly. Understanding the design implications can help buyers select products that are better suited for specific clinical situations.
Common Trade Terminology
Familiarity with industry-specific terminology is essential for effective communication and procurement. Here are some key terms:
-
OEM (Original Equipment Manufacturer)
This term refers to companies that produce parts or equipment that may be marketed by another manufacturer. In the context of dental implants, knowing your OEM can ensure product quality and reliability. -
MOQ (Minimum Order Quantity)
MOQ is the smallest quantity of a product that a supplier is willing to sell. Understanding MOQs helps buyers plan their inventory and cash flow effectively, especially in markets where demand may fluctuate. -
RFQ (Request for Quotation)
An RFQ is a document sent to suppliers requesting a quote for specific products or services. This is crucial for buyers to obtain competitive pricing and understand the terms of sale, which can vary significantly in international markets. -
Incoterms (International Commercial Terms)
These are standardized terms used in international trade to clarify the responsibilities of buyers and sellers. Familiarity with Incoterms (like FOB, CIF, etc.) is essential for understanding shipping costs, insurance, and risk transfer, particularly for international B2B transactions. -
Regulatory Compliance
This refers to adherence to laws and regulations governing medical devices in specific markets. For dental implants, compliance with local standards (like the FDA in the U.S. or CE marking in Europe) ensures that products meet safety and efficacy requirements, which is vital for building trust with healthcare providers. -
Warranty Period
This term indicates the duration for which a manufacturer guarantees the performance of an implant. Understanding warranty terms helps buyers assess product reliability and the potential for future liabilities.
By grasping these technical properties and industry terms, international B2B buyers can make informed decisions, ensuring that they procure high-quality dental implants that meet their market’s needs.
Navigating Market Dynamics, Sourcing Trends, and Sustainability in the dental implants with bone loss Sector
Market Overview & Key Trends
The global market for dental implants, particularly for patients with bone loss, is experiencing significant growth, driven by an increasing aging population and rising awareness of oral health. In regions such as Africa, South America, the Middle East, and Europe, the demand for advanced dental solutions is intensifying. Key drivers include a higher prevalence of periodontal diseases and the growing trend towards aesthetic dentistry, which emphasizes the importance of restoring not just function but also appearance.
Emerging technologies, such as 3D printing and digital implantology, are revolutionizing the sourcing and production of dental implants. These innovations enable customized solutions tailored to individual patient needs, enhancing the precision and success rates of implant procedures. For B2B buyers, this means sourcing from suppliers that leverage these technologies can provide competitive advantages in terms of quality and turnaround times.
International buyers should also consider the shift towards minimally invasive procedures, such as mini dental implants and zygomatic implants, which require less bone density and reduce recovery times. This trend opens new avenues for dental practices to cater to patients who previously might have been ineligible for traditional implants due to significant bone loss. Understanding these market dynamics is crucial for B2B buyers looking to align their offerings with current and future demand.
Sustainability & Ethical Sourcing in B2B
Sustainability has become a cornerstone of modern business practices, and the dental implants sector is no exception. The environmental impact of dental manufacturing processes, from resource extraction to waste generation, is prompting buyers to seek out suppliers committed to sustainable practices. Ethical sourcing is not merely a trend; it is becoming a necessity for businesses aiming to enhance their brand reputation and comply with increasing regulatory demands.
B2B buyers should prioritize suppliers who demonstrate a commitment to sustainability through certifications like ISO 14001 (Environmental Management) and use of eco-friendly materials. For instance, sourcing implants made from biocompatible materials that minimize ecological footprints is gaining traction. Additionally, manufacturers that engage in recycling programs or utilize renewable energy sources in their production processes are increasingly preferred.
Moreover, the importance of ethical supply chains cannot be overstated. Buyers should assess the labor practices and environmental policies of their suppliers, ensuring that they align with their corporate social responsibility goals. This not only helps mitigate risks associated with unethical sourcing but also appeals to a growing consumer base that values transparency and sustainability.
Brief Evolution/History
The evolution of dental implants has been marked by significant advancements in technology and materials. Initially, dental implants were rudimentary, often made from non-biocompatible materials. However, the introduction of titanium in the 1960s transformed the industry, as it demonstrated excellent integration with bone and longevity.
As understanding of bone loss and its implications for dental health grew, so did the innovations in implant technology. The development of bone grafting techniques and minimally invasive procedures expanded the possibilities for patients with bone loss, making implants accessible to a wider demographic. Today, the focus is not only on functionality but also on aesthetics and patient comfort, reflecting broader trends in healthcare towards personalized and patient-centered solutions. This historical context is essential for B2B buyers to appreciate the rapid advancements and ongoing potential in the dental implants market, particularly for those addressing the challenges posed by bone loss.
Related Video: Dentures, Implants, and Bone Loss
Frequently Asked Questions (FAQs) for B2B Buyers of dental implants with bone loss
-
What should I consider when vetting suppliers for dental implants with bone loss?
When vetting suppliers, prioritize their certifications and compliance with international standards such as ISO and CE marking. Assess their experience in producing implants specifically for patients with bone loss, as this requires specialized knowledge. Request references or case studies that showcase their success in similar markets. Additionally, evaluate their customer service and support capabilities, especially regarding after-sales service and product guarantees. -
Can I customize dental implants for specific patient needs?
Yes, many manufacturers offer customization options for dental implants, especially for patients with unique anatomical challenges due to bone loss. Discuss with your supplier the possibility of modifying dimensions, materials, or surface treatments to suit specific cases. Ensure that the customization process is clearly defined in the contract, including timelines and costs associated with bespoke orders. -
What are typical minimum order quantities (MOQs) and lead times for dental implants?
MOQs for dental implants can vary widely among suppliers, typically ranging from 10 to 50 units. Lead times often depend on the complexity of the order and the supplier’s production capabilities, generally taking 4 to 12 weeks. It is advisable to negotiate MOQs and establish lead times upfront to align with your inventory needs and patient demand, especially in regions with fluctuating market conditions. -
What payment options are available for international purchases of dental implants?
Most suppliers accept various payment methods, including bank transfers, credit cards, and letters of credit, which provide additional security for both parties. Discuss payment terms early in the negotiation to avoid misunderstandings. Some suppliers may offer discounts for early payments or bulk orders, which can be beneficial in managing cash flow effectively. -
How can I ensure quality assurance and certification of dental implants?
Request documentation that verifies compliance with international quality standards, such as ISO 13485 for medical devices. Suppliers should provide certificates of analysis (CoA) and quality control reports for each batch of implants. Additionally, inquire about their quality management system and any third-party audits they undergo to ensure consistent quality in their products. -
What logistics considerations should I be aware of when sourcing dental implants internationally?
Logistics plays a crucial role in international sourcing. Confirm the supplier’s capability to handle customs clearance and freight forwarding to your region. Assess shipping times and costs, as well as the potential for delays due to customs inspections. It’s also prudent to discuss insurance options for valuable shipments to safeguard against loss or damage during transit. -
How can disputes over product quality or delivery be resolved?
To mitigate disputes, establish clear terms in your contract regarding quality expectations, delivery timelines, and penalties for non-compliance. Include a clause for dispute resolution, such as mediation or arbitration, which can be less costly and time-consuming than litigation. Maintain open communication with your supplier to address any concerns promptly, fostering a collaborative approach to problem-solving. -
Are there specific regulations I need to be aware of when importing dental implants?
Yes, each country has its own regulations regarding the importation of medical devices. Familiarize yourself with the regulatory requirements in your region, such as registration with health authorities or obtaining import permits. Ensure that the implants you source meet local safety and efficacy standards. Consulting with a local regulatory expert can provide valuable insights and help navigate the complexities of compliance.
Important Disclaimer & Terms of Use
⚠️ Important Disclaimer
The information provided in this guide, including content regarding manufacturers, technical specifications, and market analysis, is for informational and educational purposes only. It does not constitute professional procurement advice, financial advice, or legal advice.
While we have made every effort to ensure the accuracy and timeliness of the information, we are not responsible for any errors, omissions, or outdated information. Market conditions, company details, and technical standards are subject to change.
B2B buyers must conduct their own independent and thorough due diligence before making any purchasing decisions. This includes contacting suppliers directly, verifying certifications, requesting samples, and seeking professional consultation. The risk of relying on any information in this guide is borne solely by the reader.
Strategic Sourcing Conclusion and Outlook for dental implants with bone loss
In navigating the complexities of sourcing dental implants for patients with bone loss, international buyers must prioritize strategic partnerships and robust supply chains. The increasing prevalence of bone loss due to various factors underscores the need for innovative solutions like bone grafting, mini implants, and zygomatic implants. Understanding these options allows buyers to meet the diverse needs of their markets, particularly in regions such as Africa, South America, the Middle East, and Europe.
Key takeaways include the importance of evaluating the quality and reliability of suppliers, considering the latest advancements in implant technology, and ensuring compliance with local regulations. By aligning procurement strategies with the latest industry trends, buyers can enhance patient outcomes and expand their market presence.
As the dental implant market continues to evolve, staying informed about emerging technologies and treatment options will be crucial. Investing in education and training for dental professionals in your region can drive adoption and foster trust in the solutions offered. Take action today to secure your position as a leader in providing effective dental solutions and improve the quality of life for patients suffering from the effects of bone loss.
