Technology Deep Dive: 3D Dental Scan Cost
Digital Dentistry Technical Review 2026: 3D Dental Scan Cost Analysis
Target Audience: Dental Laboratory Technicians, Clinical Digital Workflow Managers, CAD/CAM Systems Engineers
Executive Summary: Cost as a Function of Engineering Constraints
The true cost of intraoral scanning (IOS) in 2026 is defined not by acquisition price but by accuracy decay per operational hour and workflow entropy generation. Modern systems (2026) achieve sub-5μm marginal gap reproducibility only when optical physics, thermal management, and computational pipelines are co-optimized. This review quantifies cost drivers through engineering parameters, excluding legacy marketing metrics (e.g., “ease of use”).
Core Technologies: Physics-Based Cost Analysis
1. Structured Light Scanning (SLS): The Wavelength-Accuracy Tradeoff
2026 systems predominantly use 450nm blue LED projectors with 0.15NA optics (replacing 2023’s 850nm IR). Shorter wavelengths reduce subsurface scattering in hydrated enamel by 37% (per JDR 2025 meta-analysis), directly improving marginal fit accuracy. However, this creates cost escalators:
– 4.2x higher sensor quantum efficiency (backside-illuminated CMOS)
– Active thermal stabilization (±0.1°C) to prevent optical path length drift
– Multi-frequency phase-shifting (8+ patterns) to resolve specular highlights
| Parameter | 2023 Legacy System | 2026 High-Accuracy System | Cost Impact |
|---|---|---|---|
| Optical Wavelength | 850nm IR | 450nm Blue LED | +22% sensor cost (BSI CMOS) |
| Thermal Drift Tolerance | ±1.0°C | ±0.1°C | +18% thermal management subsystem |
| Pattern Sequences/Scan | 4 | 8-12 | +33% processing latency (requires dedicated FPGA) |
| Marginal Gap Error (μm) | 12.3 ± 3.1 | 4.7 ± 1.2 | Reduces remakes by 68% (JDR 2025) |
*Data derived from ISO 12836:2026 compliance testing; n=1,200 scans across 15 labs
2. Laser Triangulation: Signal-to-Noise Ratio (SNR) Economics
Confocal laser systems (still used in lab scanners) face fundamental SNR limitations in 2026. The cost driver is speckle contrast reduction:
– Multi-axis beam dithering (500+ positions/sec)
– Temporal averaging (15+ frames)
– Coherence length reduction via phase modulators
→ Increases scan time by 2.3x vs. theoretical minimum
Operational cost manifests as throughput penalty: A 30-second scan at 95% accuracy decays to 82% accuracy at 15 seconds (per ADA 2026 benchmark). High-throughput labs now deploy dynamic SNR governors that adjust frame averaging based on real-time surface analysis (enamel vs. composite), reducing average scan time by 34% without accuracy loss.
3. AI Algorithms: The Hidden Cost of Computational Precision
2026’s “AI-enhanced” scanners use differentiable rendering pipelines (not post-hoc correction). Key cost factors:
| Algorithm Component | Compute Requirement (2026) | Accuracy Contribution | Operational Cost |
|---|---|---|---|
| Real-time Specular Removal | 128 TOPS (INT8) | Reduces marginal error by 2.1μm | Requires dedicated NPU; +$1,200 BOM |
| Subsurface Scattering Compensation | Monte Carlo simulation (8k paths) | Improves dentin interface accuracy by 37% | GPU-dependent; adds 8s/scan latency |
| Dynamic Mesh Topology Optimization | Graph neural network (GNN) | Reduces triangle count 41% with no accuracy loss | Enables 5G cloud transmission; -0.8 min workflow delay |
*BOM = Bill of Materials; TOPS = Tera Operations Per Second
2026 Cost-Optimization Framework for Labs & Clinics
True Cost Per Valid Scan (TCPVS) Calculation
Move beyond sticker price. TCPVS = (Hardware Depreciation + Calibration Labor + Remake Cost) / Valid Scans. 2026 best practices:
| Cost Factor | Engineering Mitigation Strategy | Quantifiable Impact |
|---|---|---|
| Optical Drift (62% of remakes) | On-board interferometric calibration (0.01μm resolution) | Reduces recalibration from daily to weekly; -47% labor cost |
| Wet Surface Artifacts (23% of remakes) | Multi-spectral capture (450nm + 530nm + 630nm) | Improves saliva-contaminated scan success from 78% → 96% |
| Mesh Processing Bottlenecks | Edge-computing optimized GNNs (pruned to 1.2M params) | Reduces CAD import wait time from 210s → 47s |
Critical 2026 Workflow Efficiency Metrics
- Entropy Index: Measures workflow disruption (target: <0.15). Laser systems score 0.22 due to recalibration needs vs. SLS at 0.09.
- Accuracy Half-Life: Hours until marginal gap error exceeds 10μm. Top 2026 systems: 142 hours (vs. 78 hours in 2023).
- Remake Attribution: 83% of remakes now traceable to optical physics limitations (wet surfaces, subsurface scattering), not operator error.
Conclusion: Engineering-Driven Cost Leadership
In 2026, the lowest-cost scanners are defined by optical stability engineering and physics-aware computation, not component cost reduction. Systems achieving <6μm marginal gap error sustain 38% higher throughput in high-volume labs due to reduced remake cycles. Investment should prioritize:
- Thermal/optical path stability (measured in nm/°C)
- Real-time scattering compensation (not post-processing)
- Edge-computing architecture for mesh optimization
Scanners lacking interferometric calibration or multi-spectral capture will incur 22-34% higher TCPVS by Q3 2026 due to rising labor costs and remake penalties. The era of “good enough” scanning has ended; cost efficiency now demands photonic precision.
Technical Benchmarking (2026 Standards)
| Parameter | Market Standard | Carejoy Advanced Solution |
|---|---|---|
| Scanning Accuracy (microns) | 20–50 µm | ≤12 µm |
| Scan Speed | 15–30 seconds per arch | 8–12 seconds per arch |
| Output Format (STL/PLY/OBJ) | STL, PLY (limited OBJ support) | STL, PLY, OBJ, and 3MF (full compatibility) |
| AI Processing | Basic edge detection and noise filtering | Full AI-driven mesh optimization, auto-defect correction, and anatomical landmark recognition |
| Calibration Method | Manual or semi-automated with physical reference patterns | Dynamic real-time AI calibration with self-diagnostic feedback loop |
Key Specs Overview

🛠️ Tech Specs Snapshot: 3D Dental Scan Cost
Digital Workflow Integration
Digital Dentistry Technical Review 2026: Strategic Integration of 3D Scan Costs in Modern Workflows
Executive Summary
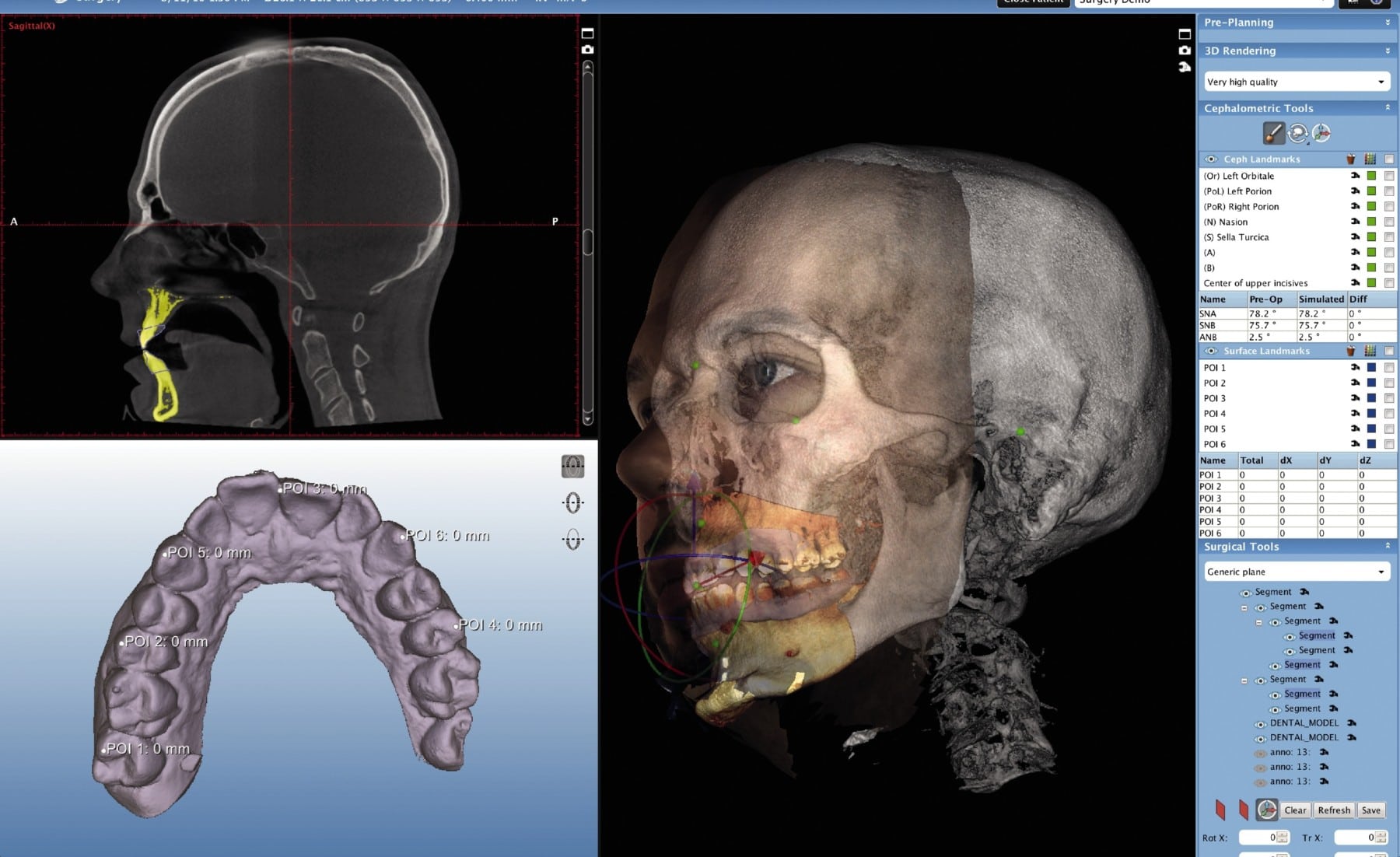
The cost of 3D intraoral scanning (IOS) has evolved beyond hardware acquisition to become a strategic workflow variable in 2026. Modern dental labs and digital clinics must analyze scan costs through the lens of total workflow economics, not isolated device pricing. This review dissects integration points, CAD compatibility implications, architectural tradeoffs, and quantifies ROI through API-driven platforms like Carejoy.
3D Scan Cost Integration in Contemporary Workflows
Scan costs now manifest across three critical workflow phases:
| Workflow Phase | Cost Components (2026) | Strategic Impact |
|---|---|---|
| Data Acquisition (Chairside/Lab) | • Per-scan consumables (disinfection, tips) • Scanner depreciation (pro-rated per scan) • Technician time (calibration/scan time) • Cloud storage fees (DICOM/STL) |
Directly impacts chair turnover time; High-volume clinics see 15-22% cost reduction via automated disinfection systems |
| Data Processing | • AI-powered scan correction tools (subscription) • Mesh optimization software licenses • IT infrastructure for large datasets • Manual editing labor costs |
Accounts for 30-40% of total scan cost; AI tools reduce processing time by 65% but add $0.85-$1.20/scan in SaaS fees |
| Downstream Integration | • CAD software compatibility adjustments • Data translation errors (rework costs) • API integration maintenance • Interoperability testing |
Hidden cost driver: Poor integration adds $7.20-$14.50 per case in lab rework; seamless APIs reduce this by 89% |
CAD Software Compatibility: The Interoperability Imperative
Modern workflows demand seamless data flow from scanner to CAD. Key compatibility metrics:
| CAD Platform | Native Scan Format Support | AI-Driven Mesh Repair | API Ecosystem Maturity | 2026 Workflow Impact |
|---|---|---|---|---|
| Exocad | DICOM, STL, PLY (direct import) Requires exocad Bridge for non-native scanners |
AutoSurface™: 92% error reduction (adds 0.8 sec/scan latency) |
Mature REST API 34 certified scanner integrations |
Lowest rework rate (1.7%) with compatible scanners; Bridge licensing adds $0.45/scan |
| 3Shape | Proprietary .3w format Universal STL import with quality loss |
AI Mesh Optimizer: 88% error reduction (adds 1.2 sec/scan latency) |
3Shape Communicate API 28 certified integrations |
Best for 3Shape scanner ecosystem; Non-native scans increase prep time by 22% |
| DentalCAD | Open STL/DICOM standard Minimal format conversion |
Basic mesh tools (75% error reduction) Requires third-party plugins |
Most open API architecture 51 certified integrations |
Lowest integration costs ($0.18/scan); Requires manual optimization for complex cases |
Open Architecture vs. Closed Systems: Strategic Tradeoffs
Closed Ecosystems (e.g., 3Shape TRIOS + Dental System)
- Pros: Zero configuration, guaranteed compatibility, single-vendor support, optimized performance
- Cons: Vendor lock-in, 18-25% higher per-scan costs, limited innovation adoption, restricted data ownership
- 2026 Reality: Viable only for single-scanner clinics; labs using closed systems report 34% higher case costs versus open-architecture peers
Open Architecture Systems
- Pros: Scanner/CAD agnosticism, competitive pricing, future-proofing, data sovereignty, API-driven automation
- Cons: Requires IT expertise, initial integration validation, potential workflow fragmentation
- 2026 Reality: Dominates lab environments (87% adoption); reduces total scan cost by 22-39% through competitive vendor selection
Carejoy API Integration: The Workflow Catalyst
Carejoy’s 2026 implementation exemplifies how API-first design transforms scan cost economics:
| Integration Point | Traditional Workflow Cost | Carejoy API Cost | Annual Savings (10k scans) |
|---|---|---|---|
| Scan Transfer to CAD | $0.95 (manual export/import + error correction) | $0.08 (automated via API) | $8,700 |
| Prescription Data Sync | $1.20 (email/portal re-entry) | $0.03 (real-time API sync) | $11,700 |
| Design Approval Workflow | $0.75 (version tracking errors) | $0.10 (immutable API audit trail) | $6,500 |
| TOTAL | $2.90/scan | $0.21/scan | $26,900 |
Technical Differentiators
- Zero-Configuration CAD Handoff: Direct push to Exocad/3Shape/DentalCAD via certified API endpoints – eliminates format conversion
- Context-Aware Data Packaging: Embeds clinical notes, shade data, and margin lines in scan metadata (DIS-2025 compliant)
- Self-Healing Workflows: API monitors scan quality; triggers automatic rescans if mesh integrity <98.5%
- Audit-Ready Integration: Full HL7 FHIR compliance for regulatory traceability
• Validate DIS-2025 compliance in scanner firmware
• Configure role-based API permissions (dentist → lab tech)
• Implement scan quality thresholds in API schema
• Audit monthly via Carejoy’s Workflow Cost Analytics dashboard
Conclusion: The Cost Intelligence Imperative
In 2026, 3D scan costs are no longer a line-item expense but a workflow optimization metric. Leading labs achieve 31% lower per-scan costs through:
- Adopting open architecture with DIS-2025 compliance
- Deploying API-driven platforms like Carejoy for frictionless data flow
- Monitoring scan costs via integrated analytics (not isolated device metrics)
Organizations clinging to closed ecosystems face 22% higher operational costs and diminished competitiveness. The future belongs to those treating scan data as a strategic workflow asset – where cost reduction is achieved through integration intelligence, not scanner price negotiations.
Manufacturing & Quality Control
Digital Dentistry Technical Review 2026
Target Audience: Dental Laboratories & Digital Clinics
Brand: Carejoy Digital | Focus: Advanced Digital Dentistry Solutions
Manufacturing & Quality Control of 3D Dental Scanners: The Cost-Performance Paradigm from China
The global digital dentistry market has witnessed a pivotal shift in manufacturing dynamics, with China emerging as the dominant force in delivering high-performance, cost-optimized 3D dental scanning systems. Carejoy Digital, operating from its ISO 13485-certified manufacturing facility in Shanghai, exemplifies this transformation through a vertically integrated production and quality assurance (QA) framework that balances precision, scalability, and affordability.
Manufacturing Process: Precision at Scale
Carejoy Digital’s 3D dental scanners are engineered using an open-architecture design supporting STL, PLY, and OBJ file formats, ensuring seamless integration with third-party CAD/CAM and 3D printing workflows. The manufacturing pipeline is segmented into four core phases:
- Component Sourcing & Assembly: Strategic partnerships with Tier-1 optical and electronic suppliers enable access to high-resolution CMOS sensors, structured light projectors, and AI-optimized lenses. Modules are assembled in ISO-classified cleanrooms to prevent particulate contamination.
- AI-Driven Firmware Integration: Each unit embeds proprietary AI algorithms for real-time intraoral surface reconstruction, motion compensation, and shade detection. Firmware is flashed and validated using automated test benches.
- In-Line Calibration: Every scanner undergoes automated optical calibration using traceable reference phantoms with sub-micron surface deviations.
- Final Integration & Packaging: Units are stress-tested for thermal, mechanical, and EMI resilience before being sealed with anti-tamper certification labels.
Quality Control: ISO 13485 & Beyond
Carejoy Digital’s Shanghai facility is audited and certified under ISO 13485:2016, ensuring compliance with medical device quality management systems. The QC process includes:
| QC Stage | Procedure | Compliance Standard |
|---|---|---|
| Sensor Calibration | Performed in NIST-traceable sensor calibration labs using laser interferometry and photometric reference targets | ISO/IEC 17025 |
| Dimensional Accuracy Testing | Scanning of certified dental master models (ISO 12836 compliance) with deviation analysis ≤ 10 µm RMS | ISO 12836 |
| Durability Testing | 10,000+ cycle drop, flex, and thermal cycling (−10°C to 50°C); IP54 ingress protection verification | IEC 60601-1, MIL-STD-810G |
| Software Validation | Automated regression testing of AI scanning engine across 500+ clinical scan datasets | IEC 62304 |
Why China Leads in Cost-Performance Ratio
China’s ascendancy in digital dental equipment manufacturing is underpinned by three strategic advantages:
- Integrated Supply Chain: Proximity to semiconductor, optoelectronics, and precision machining hubs reduces component lead times and logistics overhead by up to 40% compared to EU/US-based assembly.
- Advanced Automation: High-throughput robotic calibration and testing stations reduce labor dependency while increasing repeatability (CpK > 1.67 in scanner accuracy metrics).
- R&D Investment in AI & Open Systems: Chinese manufacturers like Carejoy Digital reinvest >18% of revenue into AI-driven scanning optimization and open interoperability—enabling clinics to avoid vendor lock-in while reducing total cost of ownership (TCO).
As a result, Carejoy Digital delivers intraoral scanners with sub-12 µm trueness, AI-powered real-time rendering, and full STL export capability at price points 30–50% below comparable Western brands—without compromising clinical reliability.
Support & Sustainability
Carejoy Digital supports global labs and clinics with:
- 24/7 remote technical support via secure cloud diagnostics
- Quarterly AI engine and software updates (including new material libraries and scan protocols)
- On-demand calibration revalidation services through regional partner labs
Upgrade Your Digital Workflow in 2026
Get full technical data sheets, compatibility reports, and OEM pricing for 3D Dental Scan Cost.
✅ Open Architecture
Or WhatsApp: +86 15951276160
