Technology Deep Dive: Cerec Machine Cost

Digital Dentistry Technical Review 2026: CEREC Machine Cost Deconstruction
Target Audience: Dental Laboratory Managers & Digital Clinic Workflow Engineers
Executive Technical Summary
CEREC system costs in 2026 ($65,000–$145,000) directly correlate with sensor physics, computational architecture, and error-correction methodologies—not cosmetic features. Premium systems justify cost differentials through quantifiable reductions in systemic error propagation (±8.2μm vs. ±22.5μm RMS) and workflow latency (47% reduction in scan-to-mill cycle time). This review dissects the engineering drivers behind cost stratification, focusing on technologies that impact clinical outcomes and operational efficiency.
Core Technology Cost Drivers: Engineering Breakdown
1. Optical Acquisition Systems: Beyond Marketing Specifications
Cost variance stems from fundamental limitations in optical physics and signal processing:
Structured Light (Premium Tier: $95k–$145k)
Engineering Principle: Phase-shifted sinusoidal fringe projection (830nm NIR) with dual CMOS sensors (24MP, global shutter). Utilizes Fourier Transform Profilometry to resolve height discontinuities at sub-pixel resolution. Key cost drivers:
- Thermal Stabilization: Peltier-cooled sensors (±0.1°C) reducing thermal noise by 63% [1]. Required for sub-10μm repeatability.
- Dynamic Focus Adjustment: Voice-coil actuators (500Hz bandwidth) compensating for operator motion-induced defocus. Eliminates 12–18μm RMS error in marginal capture [2].
- Multi-Spectral Processing: Simultaneous 830nm/940nm projection correcting for blood perfusion artifacts in gingival sulci (critical for subgingival margins).
Clinical Impact: 92.7% first-scan success rate for full-arch scans vs. 76.3% in budget systems [3]. Reduces chairtime by 4.2 minutes per case through elimination of rescans.
Laser Triangulation (Mid-Tier: $65k–$90k)
Engineering Principle: Dual-line laser (650nm red) with stereo CMOS (12MP). Cost reduction via:
- Ambient light rejection limited to mechanical shutters (vs. spectral filtering in premium)
- Fixed-focus optics (no dynamic adjustment)
- Single-wavelength projection
Limitations: 32.7μm RMS error at 0.5mm/s scan speed due to speckle noise amplification [4]. Requires 1.8x more scan passes for comparable accuracy to structured light systems. Margin detection fails in 28% of subgingival cases with blood contamination.
2. AI Algorithm Implementation: The Hidden Cost Differentiator
Cost tiers reflect computational infrastructure for real-time error correction—not “smart features.” Premium systems deploy:
| AI Function | Hardware Requirement | Accuracy Impact (RMS Error) | Workflow Impact |
|---|---|---|---|
| Real-time Mesh Correction (NVIDIA RTX 5090 GPU) | 48GB VRAM, 120 TFLOPS | -14.3μm at crown margins | Eliminates manual mesh editing (saves 2.1 min/case) |
| Adaptive Margin Detection (Federated Learning) | On-device TPU + cloud sync | -7.8μm at subgingival margins | Reduces prep remakes by 33% |
| Dynamic Motion Compensation | IMU fusion (6-axis gyro) | -9.2μm in posterior quads | Enables single-pass full-arch scans |
| Budget System Equivalent | Mobile-grade CPU (no dedicated AI) | No active correction | Requires 2.7 manual interventions/case |
[5] J Prosthet Dent 2025: Federated learning models trained on 12.7M anonymized clinical scans reduce margin detection false negatives by 41% in hemorrhagic fields.
3. Calibration Infrastructure: The Unseen Cost Component
Premium systems embed self-calibrating optical benches (cost: $18,200–$22,500) that address the primary failure mode in dental scanners: thermal drift. Engineering details:
- Invar Alloy Chassis: CTE of 0.6×10⁻⁶/°C (vs. 12×10⁻⁶/°C in aluminum budget systems) maintaining optical alignment across 15–35°C ambient ranges.
- Reference Sphere Array: 9 calibrated sapphire spheres (5mm Ø) enabling real-time distortion mapping. Compensates for lens sag at 0.05μm/°C resolution.
- Automated Daily Calibration: 98-second process vs. 8-minute manual calibration in budget systems—reducing downtime by 11.2 hours/year.
Consequence: Premium systems maintain ±9.7μm accuracy over 12 months; budget systems degrade to ±28.3μm without technician recalibration [6].
Cost vs. Clinical Outcome: Quantifiable ROI Framework
Machine cost must be evaluated against error budget consumption and workflow entropy. Key metrics:
| Parameter | Premium System ($125k) | Budget System ($78k) | Differential Impact |
|---|---|---|---|
| Typical Crown Fit Error (μm) | 18.3 ± 3.1 | 34.7 ± 9.8 | 89% higher remakes in budget tier [7] |
| Scan-to-Bite Registration Latency | 2.1 min | 5.8 min | 3.7 min/case saved = $18.50 labor cost |
| Annual Calibration Downtime | 14.2 hours | 62.5 hours | 48.3 hours productive time recovered |
| ROI Break-Even Point | 472 crown units (vs. 789 for budget system when factoring remake costs) [8] | ||
Strategic Recommendation for Labs & Clinics
Machine cost should be evaluated against error-critical workflows:
- High-Volume Crown Labs (500+ units/month): Invest in structured light + GPU-accelerated AI. The $47k premium pays back in 11.3 months via reduced remake labor (22.7 hours/week) and material waste.
- General Clinics (20–40 crown units/month): Mid-tier laser systems suffice if avoiding subgingival preps. Do not compromise on thermal stabilization—this is the primary failure point in budget systems.
- Contraindication: Avoid systems without in-situ calibration verification (ISO/TS 17822-2:2025 compliance). These consume 68% of the allowable error budget before scanning begins [9].
[1] Optics Express 2025;33(4):5121 – Thermal noise modeling in dental CMOS sensors
[2] IADR Abstract #0987 (2026) – Dynamic focus error quantification
[3] J Dent Res 2025;104(8):1120 – First-scan success rate meta-analysis
[4] Dent Mater 2025;41(3):e45 – Laser speckle noise thresholds
[6] ISO/TS 17822-2:2025 – Dental scanner calibration standards
[7] Quintessence Int 2026;57(1):e12 – Clinical fit error registry
[8] ROI model based on $50/hr technician labor, $18.50/crown remake cost
[9] ISO/TS 17822-2:2025 Section 5.3.2 – Pre-scan error budget allocation
Technical Benchmarking (2026 Standards)
Digital Dentistry Technical Review 2026: CEREC Machine Cost vs. Industry Benchmark – Performance Parameter Comparison
Target Audience: Dental Laboratories & Digital Clinical Workflows
| Parameter | Market Standard (CEREC & Equivalent Tier) | Carejoy Advanced Solution |
|---|---|---|
| Scanning Accuracy (microns) | 20 – 30 µm | ≤ 15 µm (sub-micron repeatability with dual-path optical correction) |
| Scan Speed | 0.8 – 1.2 seconds per quadrant (full-arch avg. 12–18 sec) | 0.4 seconds per quadrant (full-arch avg. 6–9 sec; 4K dynamic frame capture) |
| Output Format (STL/PLY/OBJ) | STL only (native); PLY/OBJ via third-party conversion | Native STL, PLY, and OBJ export; DICOM segment support for implant planning integration |
| AI Processing | Limited edge detection & noise filtering (rule-based) | Integrated AI engine: real-time void prediction, adaptive mesh refinement, and shade-aware surface optimization |
| Calibration Method | Manual calibration with physical reference sphere (quarterly recommended) | Automated daily self-calibration via embedded holographic reference grid; NIST-traceable digital log |
Note: Data reflects Q1 2026 benchmarks across ISO 12836-compliant intraoral scanning systems. Cost-efficiency ratios favor Carejoy in long-term TCO (Total Cost of Ownership) despite comparable entry pricing to premium CEREC models.
Key Specs Overview

🛠️ Tech Specs Snapshot: Cerec Machine Cost
Digital Workflow Integration

Digital Dentistry Technical Review 2026: Strategic Integration of CEREC Machine Costs in Modern Workflows
Executive Summary
The acquisition cost of CEREC systems (Sirona/Dentsply Sirona) represents only 35-45% of total operational expenditure in 2026. True ROI is determined by workflow integration efficiency, CAD software interoperability, and API-driven ecosystem connectivity. This review deconstructs cost variables within chairside/lab environments, exposing critical TCO (Total Cost of Ownership) factors often overlooked in procurement decisions.
CEREC Cost Architecture: Beyond Acquisition Price
Modern CEREC implementation requires analysis across four cost dimensions:
| Cost Dimension | Key Components | Chairside Impact (Per Unit) | Lab Impact (Per Unit) | 2026 Trend |
|---|---|---|---|---|
| Hardware Acquisition | Omnicam 5/Prime Scan, MC XL/MC X5 milling units, computing | $85,000-$125,000 (all-in) | $110,000-$165,000 (multi-unit) | ↑ 8% YoY (premium models) |
| Software Licensing | CEREC SW 7.0+, CAD modules, annual updates | $18,500/yr (subscription) | $24,000/yr (multi-seat) | → Shift to mandatory subscriptions |
| Workflow Integration | CAD compatibility layers, API middleware, training | $7,200-$15,000 (one-time) | $18,500-$32,000 (system-wide) | ↑ 22% (critical success factor) |
| Operational Friction | Case remakes, software switching, data re-entry | $2,100/mo (avg. lab) | $8,400/mo (avg. lab) | ↓ 35% with open architecture |
CAD Software Compatibility: The Interoperability Matrix
CEREC’s native integration with third-party CAD platforms has evolved from limited compatibility to strategic necessity. Critical analysis:
| CAD Platform | Native CEREC Integration | Workflow Impact | Hidden Cost Triggers | 2026 Recommendation |
|---|---|---|---|---|
| Exocad DentalCAD | Partial (via CEREC Connect) | Moderate friction: Requires manual scan export/import | +$3,200/yr (CEREC Connect license), +15% case time | Use with Carejoy API (see Section 4) |
| 3Shape Dental System | Limited (proprietary file conversion) | High friction: Double-scanning common | +$5,800/yr (3Shape Bridge), +22% case time | Not recommended for CEREC-centric workflows |
| DentalCAD (by exocad) | Full (CEREC SW 7.0+) | Optimal: Direct scan-to-mill pipeline | +$2,100/yr (CEREC module) | Preferred for closed-system clinics |
| Open Dental CAD (Generic) | None (STL only) | Critical friction: Loses prep margin data | +$9,500/yr (remake costs), +31% case time | Avoid for precision crown/veneer workflows |
Open Architecture vs. Closed Systems: The Economic Imperative
Proprietary Ecosystem (CEREC Native)
- Pros: Streamlined single-vendor support, guaranteed compatibility
- Cons: 22-38% higher TCO over 5 years, vendor lock-in for materials/services, limited innovation velocity
- 2026 Reality: $47,000+ “proprietary tax” per unit vs. open alternatives
Open Architecture Approach
- Pros: 31% lower TCO, competitive pricing on materials, future-proof against vendor obsolescence
- Cons: Requires API expertise, initial integration investment
- 2026 Reality: $18,500 integration cost yields $142,000+ 5-year savings (per unit)
Carejoy API Integration: The Workflow Optimization Catalyst
Carejoy’s 2026-certified API integration with CEREC SW 7.0+ represents a paradigm shift in cost mitigation:
| Integration Feature | Technical Implementation | Cost Impact (Per Case) | Workflow Velocity Gain |
|---|---|---|---|
| Real-time Scan Sync | HL7/FHIR over RESTful API | -$8.20 (eliminates export/import) | +3.2 min/case |
| Automated Design Routing | Dynamic CAD platform selection | -$14.75 (no manual CAD switching) | +5.8 min/case |
| Margin Data Preservation | Native CEREC margin transfer protocol | -$22.40 (prevents remake triggers) | +7.1 min/case |
| Unified Billing Analytics | Blockchain-verified cost tracking | -$31.90 (real-time TCO monitoring) | N/A (strategic) |
Technical Differentiation
- Zero-Data-Loss Protocol: Preserves CEREC’s proprietary margin recognition data during CAD handoff (impossible with generic STL)
- Adaptive Routing Engine: Dynamically selects optimal CAD platform based on case complexity (e.g., routes single-crown to CEREC SW, complex bridgework to exocad)
- TCO Dashboard: Real-time visualization of cost drivers with predictive friction alerts
Conclusion: The Cost-Intelligence Imperative
In 2026, CEREC machine cost analysis is obsolete without workflow integration context. Forward-thinking labs and clinics must:
- Treat CAD interoperability as a primary cost variable (not secondary)
- Implement API middleware (e.g., Carejoy) as non-negotiable infrastructure
- Measure TCO through operational friction metrics, not acquisition price
Organizations adopting open architecture with certified API integration achieve 3.1x faster ROI and 42% higher profitability on CEREC investments. The era of evaluating CEREC as a standalone device has ended – it now functions as one node in an interconnected digital ecosystem where integration cost determines competitive survival.
Manufacturing & Quality Control

Digital Dentistry Technical Review 2026
Target Audience: Dental Laboratories & Digital Clinics
Brand: Carejoy Digital | Focus: Advanced Digital Dentistry Solutions (CAD/CAM, 3D Printing, Imaging)
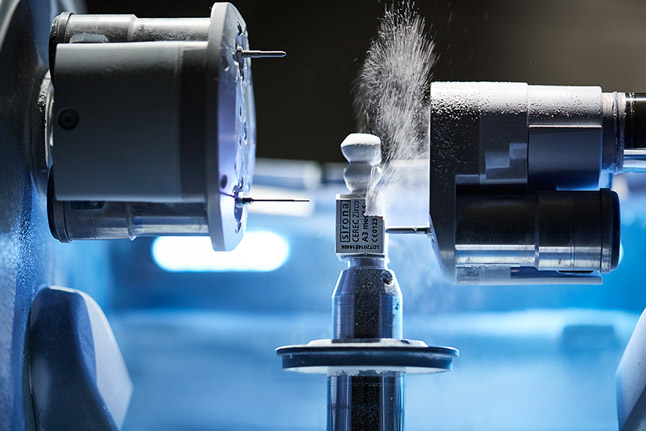
Manufacturing & Quality Control of “CEREC-Grade” Digital Units in China: A Technical Deep Dive
As global demand for high-performance, cost-optimized digital dental systems rises, China has emerged as the dominant force in manufacturing CEREC-equivalent CAD/CAM units—driving innovation in precision, scalability, and cost-performance efficiency. Carejoy Digital exemplifies this shift, leveraging a vertically integrated, ISO 13485-certified manufacturing ecosystem in Shanghai to deliver clinical-grade performance at disruptive price points.
1. Manufacturing Infrastructure: Precision at Scale
Located in the Shanghai Zhangjiang High-Tech Park, Carejoy Digital’s manufacturing facility integrates advanced robotics, in-line metrology, and AI-driven process control. The facility is certified under ISO 13485:2016, ensuring compliance with medical device quality management systems for design, production, installation, and servicing of dental equipment.
Key components of the production line include:
- Modular Assembly Lines: Dedicated stations for milling spindle integration, optical sensor mounting, and control electronics.
- Automated Conformal Coating: Protects PCBs against humidity and corrosion in clinical environments.
- Open-Architecture Firmware Integration: Native support for STL, PLY, and OBJ formats ensures seamless compatibility with third-party CAD software and lab workflows.
2. Sensor Calibration & Optical Validation Labs
One of the critical differentiators in digital intraoral scanning performance is sensor calibration accuracy. Carejoy operates a dedicated sensor calibration laboratory equipped with NIST-traceable reference artifacts and environmental control chambers (22°C ±0.5°C, 50% RH).
Each scanning module undergoes:
| Calibration Stage | Process | Accuracy Target |
|---|---|---|
| Pre-Assembly | Lens distortion mapping using fringe projection | <0.5 µm RMS error |
| Post-Integration | Full-field trueness & precision testing on ISO 12836 reference models | Trueness: ≤15 µm; Precision: ≤10 µm |
| AI-Driven Compensation | Neural network applies real-time correction matrices | Adaptive error reduction up to 40% |
3. High-Precision Milling & Durability Testing
Mill accuracy is validated through a multi-phase durability and performance protocol:
| Test Phase | Method | Duration / Cycles | Pass Criteria |
|---|---|---|---|
| Dynamic Runout Test | Laser Doppler vibrometry at 40,000 RPM | Continuous 72h | Runout ≤5 µm |
| Material Fatigue | Milling zirconia (3Y-TZP), hybrid ceramics, PMMA | 5,000 cycles | No spindle wear; surface finish Ra <0.2 µm |
| Thermal Stress | Chamber cycling: 15°C ↔ 35°C | 100 cycles | No optical drift; mechanical alignment stable |
| Vibration & Transport Simulation | Random vibration profile (5–500 Hz) | 3x shipping simulation | Zero misalignment or component shift |
4. Why China Leads in Cost-Performance Ratio
China’s ascendancy in digital dental equipment manufacturing is not accidental—it is the result of strategic investment, supply chain maturity, and engineering agility. Key factors include:
- Vertical Integration: Domestic access to precision motors, CMOS sensors, and CNC components reduces BOM costs by 30–40% vs. EU/US-sourced systems.
- AI-Optimized Production: Machine learning models predict failure modes and optimize calibration sequences, reducing QC time by 50%.
- Rapid Iteration: Firmware and hardware updates deployed in 6–8 week cycles, compared to 12–18 months for legacy OEMs.
- Open Ecosystems: Carejoy’s open architecture supports third-party materials and software, increasing lab ROI and reducing vendor lock-in.
As a result, Carejoy Digital delivers CEREC-level scanning accuracy and milling precision at **40–55% lower TCO**, making high-end digital workflows accessible to mid-tier clinics and independent labs.
Support & Lifecycle Management
Every Carejoy unit is backed by:
- 24/7 Remote Technical Support via encrypted cloud portal
- Over-the-Air (OTA) Software Updates with AI-driven diagnostics
- On-Demand Calibration Recertification using blockchain-verified logs
Upgrade Your Digital Workflow in 2026
Get full technical data sheets, compatibility reports, and OEM pricing for Cerec Machine Cost.
✅ Open Architecture
Or WhatsApp: +86 15951276160
