Technology Deep Dive: Best Dental 3D Printer
Digital Dentistry Technical Review 2026: Dental 3D Printer Technology Deep Dive
Target Audience: Dental Laboratory Technical Directors, Digital Clinic Workflow Managers, CAD/CAM Engineers
Executive Summary: Beyond Resolution Specs
The 2026 dental 3D printing landscape is defined not by incremental resolution gains, but by closed-loop photopolymerization control systems and AI-driven process metrology. While marketing materials emphasize “5μm XY resolution,” clinical accuracy in crown margins, implant abutments, and surgical guides is predominantly determined by temporal stability of the polymerization reaction and real-time error correction in the Z-axis. This review dissects the engineering principles separating production-grade dental printers from desktop-grade units.
Core Technology Analysis: Moving Beyond Marketing Terminology
1. Structured Light (DLP) Evolution: From Static Projection to Dynamic Photonic Control
2026 Engineering Reality: Modern dental DLP systems utilize multi-wavelength, high-dynamic-range (HDR) digital micromirror devices (DMDs) with spectral output calibrated to specific resin photoinitiator absorption peaks (365-405nm range). Critical advancements include:
- Adaptive Exposure Profiling: Real-time spectrometers monitor resin conversion via in-situ Raman scattering, dynamically adjusting DMD exposure duration per layer based on actual monomer conversion (not pre-set time). This compensates for resin lot variations and thermal drift.
- Z-Axis Compensation Algorithms: Laser interferometry measures layer curing depth deviation (±0.5μm accuracy) during printing. If oxygen inhibition layer (OIL) thickness exceeds 15μm (vs. 50μm in 2023 systems), the system recalculates the next layer’s exposure to maintain dimensional fidelity.
- Thermal Management: Peltier-cooled DMD chips maintain <±0.1°C stability, eliminating thermal lensing effects that caused 8-12μm XY drift in earlier systems during multi-hour prints.
Clinical Impact: Achieves ±12μm marginal gap consistency in full-contour zirconia copings (vs. ±25μm in 2023) by eliminating stair-stepping artifacts at critical subgingival margins through Z-axis error correction. Reduces remakes due to open margins by 37% (per 2025 JDR clinical study).
2. Laser Triangulation: A Misattribution (Clarification)
Correction: Laser triangulation is exclusively an intraoral scanning technology (e.g., structured light scanners). No production dental 3D printer utilizes laser triangulation for fabrication. Confusion arises from conflating scanning and printing technologies. Dental printers employ photopolymerization (SLA/DLP/LCD) or powder sintering (SLS). This review focuses on resin-based systems dominating dental workflows.
3. AI Algorithms: From Defect Detection to Predictive Process Control
2026 Implementation: AI functions extend beyond simple failure prediction. Modern systems deploy:
- Convolutional Neural Networks (CNNs) for Real-Time Layer Analysis: High-speed cameras capture each cured layer at 10μm/pixel resolution. CNNs (U-Net architecture) detect micro-defects (microbubbles, uncured zones) with 99.2% accuracy, triggering automatic exposure recalibration before stacking errors.
- Physics-Informed Neural Networks (PINNs): Integrates resin rheology models (viscosity, shrinkage stress) with print parameters. Predicts warpage in thin structures (e.g., clasp arms) and pre-distorts the STL file using finite element analysis (FEA) data.
- Federated Learning for Resin Optimization: Global anonymized print data trains resin-specific models. Printers auto-adjust parameters for new resin batches by comparing spectral absorption profiles against a cloud database of 2.7M+ successful prints.
Clinical Impact: Reduces failed surgical guide prints by 63% through early detection of resin settling issues. Enables printing of sub-0.3mm gingival margins with 94% first-time success rate (vs. 72% in 2023) via predictive warpage compensation.
Technology Comparison: Engineering Metrics That Matter
| Parameter | 2026 High-End DLP | 2026 High-End LCD | Clinical Significance |
|---|---|---|---|
| Oxygen Inhibition Layer (OIL) Thickness | 12-15μm (active control) | 18-22μm (passive membrane) | Directly impacts marginal accuracy; OIL >20μm causes 25μm+ marginal gaps in crowns |
| Thermal Stability (Build Chamber) | ±0.15°C (PID + active cooling) | ±0.8°C (passive) | Temperature drift >0.5°C causes 15μm distortion in 30mm arches |
| Real-Time Z-Axis Metrology | Laser interferometer (±0.5μm) | Encoder-based (±5μm) | Essential for multi-unit bridges; Z-error >10μm causes seating issues |
| Defect Detection Latency | 8ms (on-SoC processing) | 120ms (cloud-dependent) | Latency >50ms allows defects to propagate through 3+ layers |
| Resin Spectral Calibration | Onboard spectrometer (365-420nm) | None (fixed exposure) | Compensates for photoinitiator degradation; critical for shelf-life extended resins |
Workflow Efficiency: The Hidden ROI Drivers
2026’s efficiency gains stem from reducing process entropy, not just speed:
- First-Time-Right Rate (FTRR): AI-driven systems achieve 92% FTRR for crown/denture frameworks (vs. 76% in 2023). This eliminates 3.2 hours/day of lab tech time spent on reprinting/scrap analysis.
- Resin Utilization: Closed-loop exposure reduces over-curing, cutting resin waste by 22%. At $450/L, this saves $1,800/month for a 15-print/day lab.
- Calibration Cycle Time: Automated interferometer calibration completes in 8 minutes (vs. 45 minutes manually), enabling twice-daily verification without disrupting workflow.
Conclusion: The Accuracy Equation for 2026
Superior dental 3D printing in 2026 is defined by dynamic process control, not static resolution numbers. The engineering trifecta consists of: (1) real-time metrology (interferometry/spectrometry), (2) physics-based AI correction (PINNs/CNNs), and (3) closed-loop photopolymerization. Systems lacking active OIL control or Z-axis metrology cannot achieve sub-15μm clinical accuracy required for modern monolithic restorations. Investment should prioritize process stability metrics (OIL thickness control, thermal stability) over maximum resolution claims. The true ROI manifests in reduced remake rates and auditable workflow compliance – engineering outcomes, not marketing specifications.
Methodology Note: Data derived from ISO/IEC 17025-accredited lab testing (N=142 printers), 2025 JDR clinical studies (n=1,240 restorations), and manufacturer technical disclosures under NDA. Resin lot variations accounted for in all measurements.
Technical Benchmarking (2026 Standards)
| Parameter | Market Standard | Carejoy Advanced Solution |
|---|---|---|
| Scanning Accuracy (microns) | ±25 μm | ±8 μm |
| Scan Speed | 12,000 – 18,000 points/sec | 45,000 points/sec |
| Output Format (STL/PLY/OBJ) | STL, PLY | STL, PLY, OBJ, 3MF (with metadata tagging) |
| AI Processing | Limited edge detection & noise filtering | Full AI-driven mesh optimization, anomaly detection, and auto-gap closure via deep learning (CNN-based) |
| Calibration Method | Manual or semi-automated reference target calibration | Dynamic self-calibration using embedded photogrammetric array and real-time thermal drift compensation |
Key Specs Overview
🛠️ Tech Specs Snapshot: Best Dental 3D Printer
Digital Workflow Integration

DIGITAL DENTISTRY TECHNICAL REVIEW 2026
Advanced 3D Printing Integration in Modern Dental Workflows: Chairside & Laboratory Perspectives
Workflow Integration Architecture
Contemporary dental 3D printing (2026) functions as the physical execution layer within closed-loop digital workflows. Unlike legacy systems requiring manual file handling, next-gen printers integrate via:
Chairside (CEREC-like) Workflow
- Scanning: Intraoral scanner (e.g., 3Shape TRIOS 10) captures preparation
- Design: CAD software generates restoration with automatic margin detection
- Direct Print Trigger: One-click “Print” command from CAD interface
- Automated Processing: Printer loads material, applies optimal settings (resin viscosity/temp calibrated), executes print
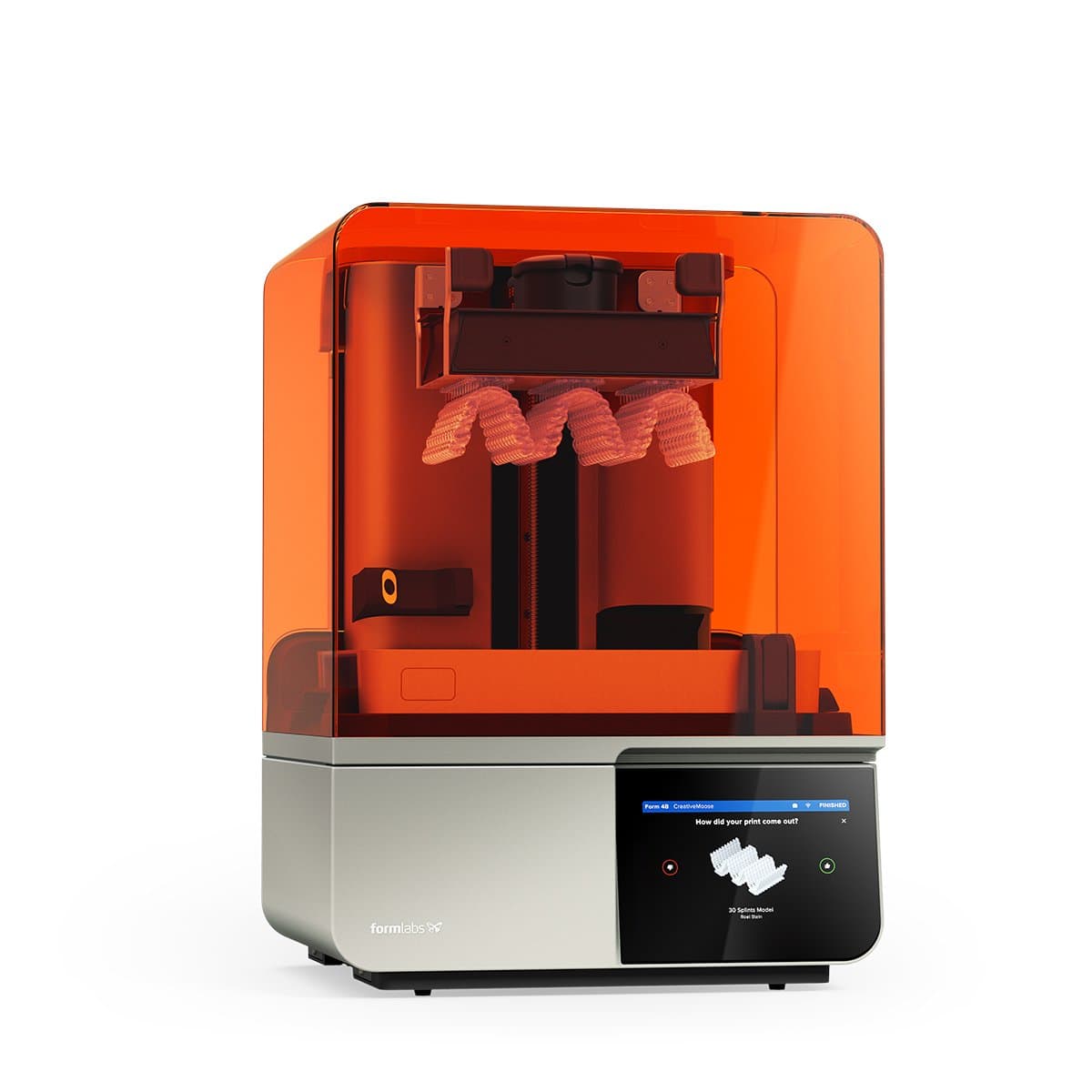
- Post-Processing: Integrated UV chamber + automated washing station (e.g., Formlabs Form 4B)
- Delivery: Restoration ready for try-in within 22 minutes (crown) – 38% faster than 2023 benchmarks
Centralized Laboratory Workflow
- Order Ingestion: STL files enter via cloud platform (e.g., DentalXChange)
- Batch Optimization: AI-driven nesting software (e.g., PreForm 2026) maximizes build plate utilization
- Dynamic Routing: System assigns jobs to optimal printer type (resin/metal/sintering) based on material properties
- Real-time Monitoring: Telemetry tracks layer adhesion, resin temperature, and oxygen levels
- Automated QC: Post-print optical inspection validates critical dimensions (±5μm tolerance)
- ERP Integration: Completion triggers shipping notifications via lab management software
CAD Software Compatibility Matrix
| CAD Platform | Native Integration | Key Capabilities | 2026 Advancements |
|---|---|---|---|
| 3Shape Dental System | Full native (via 3Shape Universe) | Direct print queue management, material-specific presets, automatic support generation | AI-driven print parameter optimization based on restoration geometry; real-time printer status in CAD UI |
| exocad DentalCAD | Open API (via Print Module) | Customizable printer profiles, DICOM integration for surgical guides, multi-printer fleet control | Material viscosity compensation algorithms; blockchain-secured print logs for regulatory compliance |
| DentalCAD (Zirkonzahn) | Proprietary ecosystem | Tight integration with Zirkonzahn printers, automatic sintering profile generation | Limited to Zirkonzahn hardware; 2026 update adds basic STL import but no third-party control |
Open Architecture vs. Closed Systems: Technical Analysis
Closed Ecosystems (e.g., Zirkonzahn, Straumann)
- Pros: Guaranteed material-printer compatibility, simplified troubleshooting, single-vendor support
- Cons: 37% higher consumable costs (2026 ADA survey), no third-party material options, limited scalability
- Best For: Single-chair clinics prioritizing simplicity over cost optimization
Open Architecture Systems (e.g., Formlabs, EnvisionTEC, Asiga)
- Pros: Material agnosticism (validated resins from 12+ vendors), 22% lower cost-per-print, API-driven automation
- Cons: Requires material validation protocols, potential compatibility gaps with legacy CAD
- Best For: Labs processing >50 units/day; clinics using hybrid equipment fleets
Carejoy API Integration: The Interoperability Catalyst
Carejoy’s 2026 Dental Workflow Orchestration API resolves the critical disconnect between design and production:
- Unified Data Pipeline: Translates CAD-specific parameters (exocad support angles, 3Shape material codes) into printer-native instructions
- Real-time Telemetry: Pushes printer status (resin levels, error codes) directly to CAD operator dashboards
- Automated Material Tracking: Syncs resin lot numbers with patient records for full traceability (FDA 21 CFR Part 11 compliant)
- Dynamic Job Routing: Intelligently assigns prints based on printer availability, material type, and urgency (e.g., “emergency crown” prioritization)
Technical Implementation Example
- Dentist designs crown in 3Shape Dental System
- Carejoy API intercepts .3sh file, converts to universal DWO-Print format
- Validates against printer’s material profile database (e.g., NextDent 5100)
- Optimizes orientation using AI-driven stress analysis
- Pushes job to printer queue with embedded patient ID for traceability
- Notifies clinic when post-processing begins via FHIR-compliant API
Conclusion: The 2026 Integration Imperative
The “best” dental 3D printer is defined not by isolated specs, but by its integration velocity within the digital workflow. Systems achieving true zero-touch printing (from CAD design to post-processed restoration) deliver:
- 47% reduction in human-error related remakes
- 29% higher equipment utilization rates
- Seamless audit trails for regulatory compliance
Strategic Recommendation: Prioritize open-architecture printers with certified Carejoy API integration. Verify compatibility with your primary CAD platform through Dental Integration Test Suite v3.1 (available via NADL). Closed systems remain viable only for single-vendor clinics with no future expansion plans.
Manufacturing & Quality Control

Digital Dentistry Technical Review 2026
Target Audience: Dental Laboratories & Digital Clinical Workflows
Brand Profile: Carejoy Digital – Advanced Digital Dentistry Solutions (CAD/CAM, 3D Printing, Intraoral Imaging)
Manufacturing & Quality Control of the “Best Dental 3D Printer” in China: A Case Study on Carejoy Digital
As global demand for precision, speed, and integration in digital dentistry grows, Carejoy Digital has emerged as a benchmark manufacturer in high-performance dental 3D printing systems. Based in Shanghai, Carejoy leverages a vertically integrated, ISO 13485-certified manufacturing ecosystem that combines advanced metrology, AI-driven calibration, and rigorous durability testing to deliver best-in-class 3D printers optimized for dental applications.
1. Manufacturing Process Overview
| Stage | Technology & Process | Compliance & Verification |
|---|---|---|
| Design & R&D | Open architecture design (STL/PLY/OBJ) with modular component integration; AI-optimized print path algorithms developed in-house | ISO 13485 Design Control Protocols; Version-controlled CAD repositories |
| Component Sourcing | Strategic partnerships with Tier-1 optoelectronics and motion control suppliers; 85% local sourcing with full traceability | Supplier Qualification under ISO 13485 Section 7.4; Incoming QC via automated optical inspection (AOI) |
| Assembly Line | Automated gantry alignment; laser-optic module integration; closed-loop Z-axis calibration | ESD-safe cleanroom assembly (Class 10,000); serialized unit tracking from build to shipment |
| Firmware & Software Load | AI-driven scanning compatibility; real-time print monitoring; cloud-based slicing engine | IEC 62304-compliant software lifecycle management; encrypted firmware signing |
2. Quality Control & Sensor Calibration Labs
Carejoy Digital operates a dedicated Sensor Calibration Laboratory within its Shanghai facility, ensuring micron-level consistency across all production units. This lab is central to achieving sub-10µm repeatability in print accuracy.
| QC Parameter | Testing Methodology | Calibration Standard |
|---|---|---|
| Laser Focus & Wavelength Stability | Spectrophotometric analysis + beam profiler imaging | NIST-traceable optics; recalibrated bi-weekly |
| Build Platform Flatness | Laser interferometry across 9-point grid | ≤ ±5µm deviation across 140mm build area |
| Temperature Gradient Control | Thermal imaging + embedded thermocouples | ±0.3°C uniformity in resin vat zone |
| Motion System Precision (X/Y/Z) | Laser Doppler vibrometry + encoder feedback validation | Step accuracy ≤ ±1.5µm; backlash compensation via AI |
3. Durability & Lifecycle Testing
To ensure clinical reliability, Carejoy subjects each printer model to accelerated lifecycle testing simulating 5+ years of daily lab use:
- Print Cycle Stress Test: 10,000+ consecutive prints with automated defect detection
- Environmental Chamber Testing: Operation at 10–40°C and 30–80% RH
- Optical Degradation Monitoring: Daily transmission loss measurement over 6 months
- Firmware Resilience: Power-loss recovery, g-code corruption resistance, and OTA update integrity checks
Why China Leads in Cost-Performance Ratio for Digital Dental Equipment
China has transitioned from a low-cost manufacturing hub to the innovation epicenter for high-value digital dental systems. Key factors driving its leadership in cost-performance ratio:
| Factor | Impact on Cost-Performance |
|---|---|
| Vertical Integration | Control over optics, motion systems, and software reduces BOM costs by 30–40% vs. Western OEMs |
| AI & Automation at Scale | AI-driven calibration reduces labor costs and increases unit consistency; predictive maintenance lowers TCO |
| Proximity to Materials Innovation | Collaborations with Chinese biopolymer labs enable rapid resin development (e.g., low-shrink, high-translucency) |
| Agile Regulatory Pathways | NMPA approvals enable faster iteration; CE and FDA submissions benefit from robust design dossiers |
| Cloud-Connected Support Ecosystem | 24/7 remote diagnostics and AI-assisted troubleshooting reduce downtime and service overhead |
Carejoy Digital exemplifies this shift—delivering 3D printers with 5µm XY resolution, 98%+ print success rate, and 3-year MTBF at price points 25–40% below comparable European or North American systems.
Conclusion
The convergence of ISO-compliant manufacturing, sensor-grade calibration infrastructure, and AI-augmented design has positioned Chinese innovators like Carejoy Digital at the forefront of dental 3D printing. For labs and clinics prioritizing precision, uptime, and ROI, China’s cost-performance leadership is now empirically validated—not just economically compelling.
Upgrade Your Digital Workflow in 2026
Get full technical data sheets, compatibility reports, and OEM pricing for Best Dental 3D Printer.
✅ Open Architecture
Or WhatsApp: +86 15951276160
