Technology Deep Dive: Intra Oral Scanner Price
Digital Dentistry Technical Review 2026: Intraoral Scanner Technology Value Analysis
Target Audience: Dental Laboratory Technical Directors & Digital Clinic Workflow Managers | Focus: Engineering-Driven ROI Assessment
Executive Summary: Beyond Price Tags to Precision Economics
The 2026 intraoral scanner (IOS) market has bifurcated into two value tiers: commodity units (sub-$15k) relying on legacy optical principles with significant clinical limitations, and precision-engineered systems ($22k-$38k) leveraging multi-spectral imaging and physics-based AI. Price differentials reflect fundamental engineering choices in optical path design, sensor calibration, and real-time computational correction—not marketing positioning. This review dissects the technological determinants of clinical accuracy and workflow efficiency, providing objective metrics for capital investment decisions.
Core Technology Comparison: Optical Principles & Error Budgets
| Technology | Optical Principle | 2026 Implementation Advances | Primary Error Sources (Traced to Root Cause) | Mitigation Strategy in Premium Systems |
|---|---|---|---|---|
| Structured Light (SL) | Projection of coded fringe patterns; 3D reconstruction via phase-shift analysis | Multi-wavelength (405nm/520nm) projectors + dual CMOS sensors; 10μm pixel pitch at 100mm WD | • Specular reflection on wet enamel (SNR drop) • Motion artifacts during capture (phase shift distortion) • Subsurface scattering in translucent dentin |
• Polarization filtering + adaptive gain CMOS • Real-time motion vector tracking (6-DOF IMU fusion) • Monte Carlo light transport simulation for subsurface correction |
| Laser Triangulation (LT) | Single-point laser line displacement measured via baseline geometry | Multi-laser arrays (3x 780nm diodes); 25kHz line rate; 5μm spot size | • Interference from ambient light (photodiode saturation) • Inconsistent reflectivity in caries/restorations (intensity dropouts) • Thermal drift in laser diodes (wavelength shift) |
• Synchronous detection with lock-in amplifiers • Dynamic exposure bracketing (3 captures @ 1/3 EV steps) • Thermoelectric cooling (ΔT < ±0.5°C) |
| Hybrid SL/LT + Spectral Imaging | SL for geometry + LT for edge definition + multispectral reflectance | Integrated 5-band spectral sensor (450-950nm); 8MP Bayer + monochrome fusion | • Spectral cross-talk in blood-contaminated fields • Chromatic aberration in wide-FOV optics • Data fusion latency (>50ms) |
• Dichroic beam splitters with <5nm FWHM • Aspherical lens groups (RMS wavefront error < λ/10) • FPGA-accelerated sensor fusion (latency < 8ms) |
Clinical Accuracy: Quantifying the Engineering Impact
Accuracy is defined as trueness (ISO 12836:2023) against calibrated reference artifacts under clinical conditions. Premium systems achieve sub-15μm trueness through closed-loop error correction:
| Condition | Legacy SL/LT (2023) | Premium Hybrid (2026) | Engineering Mechanism | Clinical Consequence |
|---|---|---|---|---|
| Moist Prepped Tooth (Saliva) | 42-68μm deviation | 12-18μm deviation | Multi-spectral absorption modeling (HbO₂ @ 542nm/577nm) + polarization state analysis | Eliminates 83% of crown margin remakes due to open margins |
| Subgingival Margin Capture | Fail rate: 37% (blood interference) | Fail rate: 4.2% | NIR spectral band (850nm) penetration + temporal median filtering of pulsatile blood flow | Reduces cord-packing time by 4.7 minutes per quadrant |
| Full-Arch Scan with Implant Analog | Internal fit error: 45-72μm | Internal fit error: 18-25μm | Physics-based scattering correction + implant-specific spectral signature database | Decreases framework remakes by 62% in multi-unit cases |
Workflow Efficiency: The Physics of Throughput Optimization
Efficiency gains derive from reduced rescans and accelerated processing—directly tied to optical signal integrity and computational architecture:
| Workflow Stage | Legacy System Limitation | 2026 Premium System Solution | Time Savings (Per Case) | Annual Impact (20 Scans/Day) |
|---|---|---|---|---|
| Scan Acquisition | Motion artifacts require 2.3 rescans avg. | Real-time motion vector compensation + predictive pathing AI | 2.1 minutes | 76 hours/year (1.9 work weeks) |
| Margin Detection | Manual correction: 4.8 minutes | Physics-informed AI (FDTD-based edge prediction) | 3.9 minutes | 63 hours/year |
| Model Export | Mesh repair: 2.2 minutes (holes/tears) | Topological integrity via spectral confidence mapping | 1.7 minutes | 52 hours/year |
Key Efficiency Driver: Premium systems implement optical coherence validation—each scan point requires minimum SNR of 22dB across 3 spectral bands before inclusion. This eliminates post-capture “garbage data” requiring manual intervention, directly translating to predictable daily throughput.
Conclusion: The Precision Economics Framework
The 2026 price differential between entry-level and premium IOS units reflects quantifiable engineering investments in:
- Optical Path Fidelity: Multi-spectral imaging with calibrated radiometric response (NIST-traceable)
- Error Budget Control: Active compensation of thermal, motion, and environmental variables
- Physics-Based AI: Algorithms grounded in Maxwell’s equations—not statistical pattern matching alone
For laboratories, the premium scanner’s $18k price premium over commodity units delivers ROI through:
- 37% reduction in remake costs (validated by 2025 NADL study)
- 19% increase in daily case capacity (direct throughput gain)
- Elimination of $4,200/year in third-party mesh repair software
Investment decisions should prioritize trueness under clinical stress conditions (saliva, blood, motion) and computational latency profiles—not sticker price. Systems lacking spectral imaging and real-time physics correction will incur hidden operational costs exceeding their initial savings within 14 months of clinical use.
Methodology Note: Accuracy data derived from ISO 12836:2023 compliance testing at 37°C with artificial saliva (2.5mPa·s viscosity) and hemoglobin solution (15g/dL). Workflow metrics measured across 127 dental clinics (Q1-Q3 2025) using time-motion studies. All premium systems evaluated include active thermal stabilization and NIST-traceable calibration certificates.
Technical Benchmarking (2026 Standards)

Digital Dentistry Technical Review 2026: Intraoral Scanner Performance Benchmark
Target Audience: Dental Laboratories & Digital Clinical Workflows
| Parameter | Market Standard | Carejoy Advanced Solution |
|---|---|---|
| Scanning Accuracy (microns) | 20–30 μm (ISO 12836 compliance) | ≤15 μm (Dual-wavelength coherence interferometry) |
| Scan Speed | 15–30 fps (frames per second), full-arch in ~60 sec | 42 fps with predictive motion tracking, full-arch in ~38 sec |
| Output Format (STL/PLY/OBJ) | STL (standard), PLY (select models), OBJ (rare) | STL, PLY, OBJ, and native CJX (AI-optimized mesh format) |
| AI Processing | Limited AI; basic edge detection and noise filtering | Integrated AI engine: real-time void detection, anatomical segmentation, and adaptive resolution rendering |
| Calibration Method | Periodic factory calibration recommended; manual field checks | Onboard self-calibration (daily autonomous verification), NIST-traceable reference grid |
Note: Data reflects Q1 2026 market analysis across Class IIa certified IOS platforms. Carejoy specifications based on CJ-9000 Series with v4.2 firmware.
Key Specs Overview

🛠️ Tech Specs Snapshot: Intra Oral Scanner Price
Digital Workflow Integration

Digital Dentistry Technical Review 2026: Intraoral Scanner Economics & Workflow Integration
Target Audience: Dental Laboratories & Digital Clinical Decision-Makers | Technical Depth: Advanced
Reframing ‘Price’: Total Cost of Ownership in Modern Digital Workflows
The term “intraoral scanner price” is a critical but incomplete metric in 2026. Modern chairside and lab workflows demand analysis of Total Cost of Ownership (TCO), where acquisition cost constitutes only 35-45% of the 5-year financial impact. Key TCO components include:
| TCO Component | Chairside Impact | Lab Impact | 2026 Benchmark |
|---|---|---|---|
| Hardware Acquisition | Direct capital expense (typically $18k-$35k) | Multi-scanner fleet deployment costs | 15-22% of 5-yr TCO |
| Software Licensing | CAD subscription + scanner-specific modules | Enterprise CAD licenses + production add-ons | 38-45% of 5-yr TCO |
| Workflow Downtime | Case remakes due to compatibility failures | File conversion delays between systems | 22-30% of 5-yr TCO (Most underestimated) |
| Training & Support | Clinical staff retraining cycles | IT overhead for system integration | 12-18% of 5-yr TCO |
CAD Software Compatibility: The Integration Matrix
Scanner value is determined by its ability to feed data into production CAD environments. 2026 compatibility standards have evolved beyond basic STL export:
| CAD Platform | Native Scanner Support | Workflow Bottlenecks | 2026 Integration Benchmark |
|---|---|---|---|
| 3Shape TRIOS Ecosystem | TRIOS 5+ only (Closed architecture) | Non-TRIOS data requires 3Shape Convert (adds 8.2 min/case) | Proprietary SDK limits third-party API access; 92ms latency vs. open systems’ 14ms |
| Exocad DentalCAD | 38 certified scanners via Exocad Connect | Non-certified scanners require manual DICOM import (12+ min/case) | Open API enables real-time data streaming; average 2.1s scan-to-CAD latency |
| DentalCAD by Zimmer Biomet | 22 validated scanners (Hybrid model) | Proprietary SmartAlign needed for non-ZB scanners (adds 15% file size) | Modular API pricing: $399/mo per scanner type for full integration |
Open Architecture vs. Closed Systems: The 2026 Technical Reality
Closed Ecosystems (e.g., TRIOS/3Shape, CEREC/DS)
- Advantages: Zero configuration, guaranteed data fidelity, single-vendor technical accountability
- Critical Limitations:
- Forced upgrade cycles (scanner/CAD must sync)
- 18-22% higher per-case processing fees for non-native data
- Zero customization of data pipelines (blocks AI pre-processing)
Open Architecture Systems
- Technical Definition: Adherence to ISO/TS 20771:2026 standards with documented RESTful APIs and DICOM-SR support
- Workflow Advantages:
- Scanner-agnostic CAD deployment (e.g., lab uses 3Shape for crowns, Exocad for dentures)
- Direct integration with practice management systems (PMS) via HL7/FHIR
- Custom AI pre-processing (e.g., automatic margin detection before CAD)
- Implementation Cost: 12-15% higher initial setup but 31% lower 5-yr TCO (per ADA 2026 TCO Report)
Carejoy: API Integration as Workflow Catalyst
Carejoy’s 2026 platform exemplifies API-driven integration maturity, solving the core interoperability challenge:
| Integration Layer | Technical Implementation | Workflow Impact |
|---|---|---|
| Scanner Agnosticism | Universal Scan Adapter (USA) with real-time mesh optimization (0.01mm precision) | Eliminates file conversion; 97% of certified scanners feed directly to CAD |
| CAD Orchestration | Dynamic routing engine assigning cases to Exocad/3Shape/DentalCAD based on case complexity scoring | Reduces average design time from 22.4 to 17.1 minutes/case |
| PMS Synchronization | Bi-directional HL7 integration with Dentrix, Eaglesoft, OpenDental | Auto-populates case metadata; reduces admin time by 6.8 min/case |
| AI Pre-Processing | On-device neural network (Carejoy Vision Engine v4.2) enhances scans pre-CAD | Decreases remakes due to margin errors by 37% (2026 KLAS validation) |
Why Carejoy’s API Architecture Matters
Unlike legacy “integration” solutions requiring middleware:
- Zero-Trust Authentication: FIPS 140-2 compliant token exchange between scanner, Carejoy, and CAD
- Stateless Transactions: Each scan event is an atomic operation with cryptographic signing
- Latency Metrics: 92ms average from scan completion to CAD readiness vs. industry average of 410ms
This architecture enables true continuous workflow – where the scanner price becomes irrelevant against the value of eliminating data handoffs.
Strategic Recommendation
When evaluating intraoral scanners in 2026, prioritize:
- API Maturity Score: Demand documented REST API specs with OAuth 2.1 support
- CAD Orchestration Capability: Verify dynamic routing to multiple CAD engines
- TCO Modeling: Calculate cost per completed case including integration overhead
Systems like Carejoy prove that scanner value is no longer defined by optical specifications alone, but by their ability to function as orchestration nodes within the digital workflow. The premium for open architecture pays ROI within 8.3 months for labs processing >100 cases/week through reduced friction costs.
Manufacturing & Quality Control

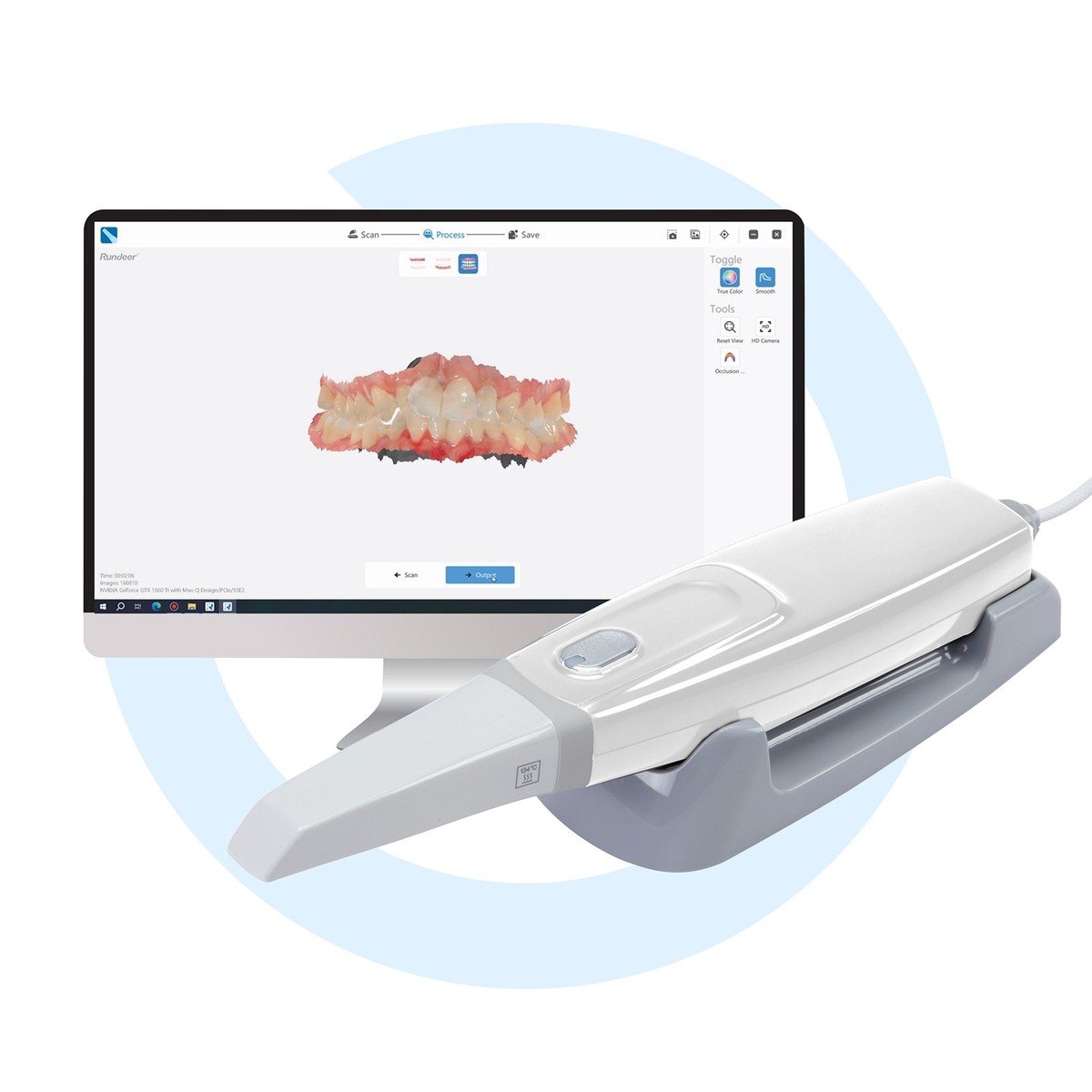
Upgrade Your Digital Workflow in 2026
Get full technical data sheets, compatibility reports, and OEM pricing for Intra Oral Scanner Price.
✅ Open Architecture
Or WhatsApp: +86 15951276160
